
Int J Curr Pharm Res, Vol 17, Issue 2, 89-92Case Study
INVASIVE DUCTAL CARCINOMA OF BREAST IN A 53 Y OLD MALE: A RARE CASE REPORT WITH LITERATURE REVIEW
PRAGNYA PARAMITA MISHRA1*, PREMANAND PANDA2
1Department of Pathology, Hi-Tech MCH, Rourkela-769004, Odisha, India. 2Department of Radiology, JP hospital and Research Centre, Rourkela, Odisha, India
*Corresponding author: Pragnya Paramita Mishra; *Email: pparamita1982@gmail.com
Received: 10 Dec 2024, Revised and Accepted: 22 Feb 2025
ABSTRACT
Male breast cancer is infrequently seen, representing less than 1% of all breast cancer cases and less than 1.5% of all cancers in men. Because of a lack of awareness, it leads to late presentation and diagnosis. Because of its rarity, very little is known about its risk factors, including hormonal and genetic anomalies. According to certain research, the distribution of tumor subtypes in male breast cancer differs from that in female breast cancer, which could indicate significant biological and prognostic variations. Larger studies need to be conducted stating which genetic abnormalities contribute to breast cancer in men and in determining which markers serve as crucial prognostic indicators. Our case is a 53-year-old male who presented with advanced-stage breast cancer with axillary lymphadenopathy in a setting of multiple neurofibromas.
Keywords: Male breast cancer, Diagnosis, Genetics, Neurofibroma, Mutation
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i2.6080 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Male breast cancer is infrequently seen, representing less than 1% of all breast cancer cases and under 1.5% of all cancers in men [1-3]. A lack of awareness often leads to late presentations and postponed diagnoses. This study was conducted to evaluate the clinical presentation, radiological findings, pathology, molecular markers, and survival rates in male breast cancer patients.
CASE REPORT
A 53 y old man was presented to our hospital with a progressively enlarging lump in his left breast with surface ulceration. He had multiple neurofibromas all over his body. Physical examination revealed a hard mass in the left breast with skin involvement and erythema of the skin. He underwent an ultrasound that revealed a large lobulated heterogeneous (fig. 1) wider-than-taller mass lesion at the 2 o'clock position in the periareolar region with posterior acoustic enhancement with pectoralis muscle infiltration and overlying skin thickening and ulceration (BIRAD V). Also, left axillary lymphadenopathy (fig. 2) was noted.
In the setting of multiple neurofibromas, the possibility of sarcoma in the setting of neurofibromas was suspected, and the patient was subjected to fine needle aspiration cytology, which showed malignant duct epithelial cells in clusters suggesting duct carcinoma of the breast. Then, the patient was subjected to a CT scan (fig. 3), which showed a soft tissue tumor in the subcutaneous plane with surface ulceration and axillary lymphadenopathy.
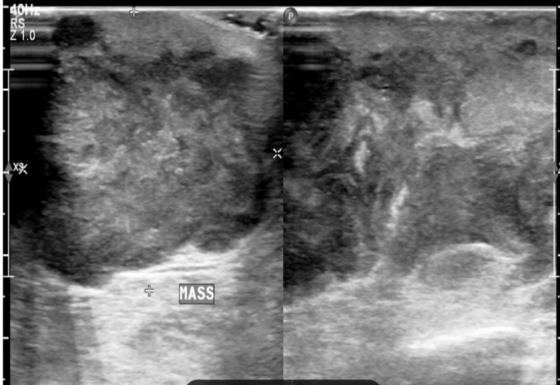
Fig. 1: Ultrasound picture showing hypoechoic lobulated mass infiltrating chest wall
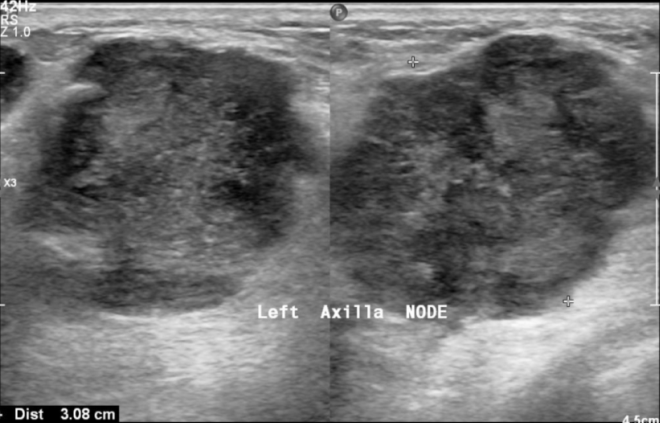
Fig. 2: Ultrasound picture showing left axillary lymphadenopathy
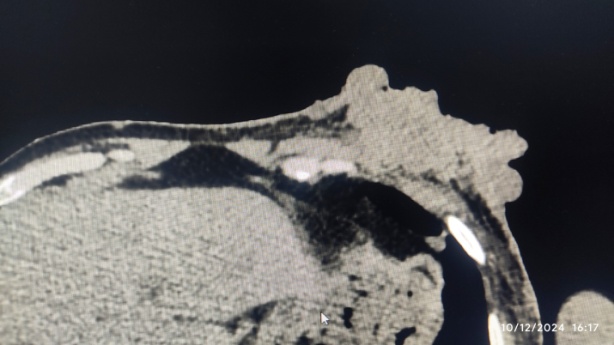
Fig. 3: CT scan showing ulcerating soft tissue lesion in left anterior chest wall infiltrating pectoralis major muscle
Then, the patient was subjected to modified radical mastectomy with axillary clearance, and a diagnosis of invasive duct carcinoma of the breast, no special type, with pT4N2aMx (fig. 4) was made.
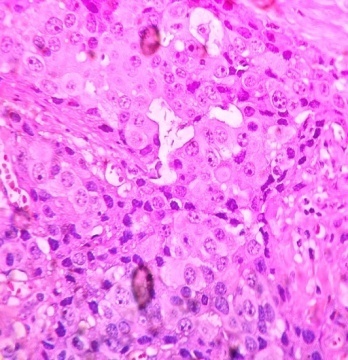
Fig. 4: H and E microphotograph showing invasive duct carcinoma cells in 40x
Immunohistochemistry showed ER (fig. 5) and PR (fig. 6) positivity with HER2neu negative status. The patient is now undergoing chemotherapy and radiotherapy and is under regular follow-up. Genetic tests for NF mutation were not done.
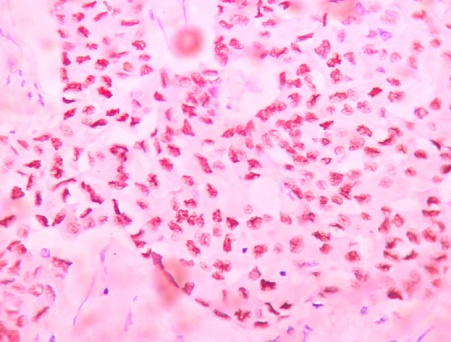
Fig. 5: Microphotograph showing invasive duct carcinoma cells are ER-positive
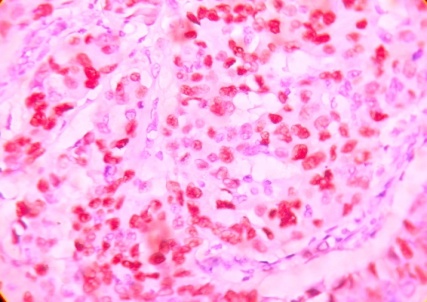
Fig. 6: Microphotograph showing invasive duct carcinoma cells are PR-positive
DISCUSSION
As male breast cancer is relatively uncommon; little is known about its genesis. However, a number of risk factors, including hormonal and genetic anomalies, have been found. Between 15% and 20% of males who have breast cancer say they have a family history of ovarian or breast cancer [4]. The most obvious gene mutation linked to breast cancer is BRCA2, and it is estimated that 10% of men with the disease have a hereditary predisposition [5]. Additionally, BRCA1 mutation has been linked to male breast cancer [6], and CHEK2 mutation has also been linked [7]. According to published reports, between 3% and 7.5% of men with breast cancer have Klinefelter's syndrome (XXY) [6].
Only 1% of male breast cancers are triple negative, 9% are HER-2 positive, 88% express androgen receptors, and the majority (88%) appear as a luminal A-like subtype. A number of diseases linked to the risk of male breast cancer are exacerbated by excess estrogen and insufficient androgens [4]. Progesterone and Estrogen levels were low in this patient, but androgen expression was not detectable.
A history of diabetes has been linked in certain studies to a modestly increased risk of male breast cancer. His breast cancer may, therefore, be exacerbated by his diabetes. Drinking alcohol has not always been linked to an increased risk of breast cancer in men. Men with localized and operable breast cancer receive the same treatment as women: systemic therapy with hormone therapy and locoregional therapy with surgery plus or minus radiation.
The overall prognosis for men with breast cancer is comparable to that of women. Similar to women with breast cancer, the condition of the axillary lymph nodes, tumor size, and stage all have a significant impact on the prognosis. The propensity for a later diagnosis may be the cause of the perception that male breast cancer has a poorer prognosis. According to certain research, the distribution of tumor subtypes in male breast cancer differ from that in female breast cancer, which could indicate significant biological and prognostic variations [8]. It has been found that males with increased levels of estrogen or decreased levels of androgens have a high chance of developing breast cancer [9]. Liver disease increases peripheral estrogen conversion from androgens, therefore predisposing to male breast cancer [10].
CONCLUSION
Male breast cancer is quite uncommon and often presents at more advanced clinical stages with a greater likelihood of lymph node involvement. In men, breast cancer tends to be more common. Hormone-receptor positive, and the BRCA2 mutation significantly increases risk. There are numerous areas for future research, and larger studies examining pathological markers would be beneficial in identifying which genetic abnormalities contribute to breast cancer in men and in determining which Markers serve as crucial prognostic indicators.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICT OF INTERESTS
Declared none
REFERENCES
Rudlowski C. Male breast cancer. Breast Care (Basel). 2008;3(3):183-9. doi: 10.1159/000136825, PMID 20824037.
Crichlow RW, Galt SW. Male breast cancer. Surg Clin North Am. 1990;70(5):1165-77. doi: 10.1016/s0039-6109(16)45237-0, PMID 2218826.
Giordano SH, Buzdar AU, Hortobagyi GN. Breast cancer in men. Ann Intern Med. 2002;137(8):678-87. doi: 10.7326/0003-4819-137-8-200210150-00013.
Sousa B, Moser E, Cardoso F. An update on male breast cancer and future directions for research and treatment. Eur J Pharmacol. 2013;717(1-3):71-83. doi: 10.1016/j.ejphar.2013.03.037, PMID 23545364.
Couch FJ, Farid LM, DE Shano ML, Tavtigian SV, Calzone K, Campeau L. BRCA2 germline mutations in male breast cancer cases and breast cancer families. Nat Genet. 1996 May;13(1):123-5. doi: 10.1038/ng0596-123, PMID 8673091.
Brose MS, Rebbeck TR, Calzone KA, Stopfer JE, Nathanson KL, Weber BL. Cancer risk estimates for BRCA1 mutation carriers identified in a risk evaluation program. J Natl Cancer Inst. 2002;94(18):1365-72. doi: 10.1093/jnci/94.18.1365, PMID 12237282.
Meijers Heijboer H, Van Den Ouweland A, Klijn J, Wasielewski M, DE Snoo A, Oldenburg R. Low penetrance susceptibility to breast cancer due to CHEK2(*)1100delC in noncarriers of BRCA1 or BRCA2 mutations. Nat Genet. 2002 May;31(1):55-9. doi: 10.1038/ng879, PMID 11967536.
Kornegoor R, Verschuur Maes AH, Buerger H, Hogenes MC, DE Bruin PC, Oudejans JJ. Molecular subtyping of male breast cancer by immunohistochemistry. Mod Pathol. 2012 Mar;25(3):398-404. doi: 10.1038/modpathol.2011.174, PMID 22056953.
Korde LA, Zujewski JA, Kamin L, Giordano S, Domchek S, Anderson WF. Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol. 2010;28(12):2114-22. doi: 10.1200/JCO.2009.25.5729, PMID 20308661.
Brinton LA, Carreon JD, Gierach GL, MC Glynn KA, Gridley G. Etiologic factors for male breast cancer in the U.S. Veterans affairs medical care system database. Breast Cancer Res Treat. 2010;119(1):185-92. doi: 10.1007/s10549-009-0379-0, PMID 19330525.