
Int J Curr Pharm Res, Vol 17, Issue 4, 94-97Original Article
COMPARISION OF ANALGESIC EFFICACY OF ROPIVACAINE VERSUS BUPIVACAINE IN ULTRASOUND GUIDED BILATERAL ERECTOR SPINAE BLOCK IN LAPAROSCOPIC CHOLECYSTECTOMY: RANDOMIZED CLINICAL TRIAL
GEETHA S. HASSARADDI1, PRATIBHA SD2*, PRASHANTH VADIGERI1, SHYNEE JN1, RAMESH BABU1
1Department of Anesthesiology and Critical Care Navodaya Medical College and Research Center, Raichur, Karnataka, India. 2Department of Anaesthesiology, Bldedu Shri B M Patil Medical College, Vijayapura-586103, Karnataka, India
*Corresponding author: Pratibha SD; *Email: pratibhakaradi@gmail.com
Received: 12 Apr 2025, Revised and Accepted: 06 Jun 2025
ABSTRACT
Objective: Laparoscopic cholecystectomy (LC) is the primary treatment for cholelithiasis and is minimally invasive surgery, but common adverse effects is post-operative pain. Our study aims to assess the analgesic effect of Erector spinae plane block (ESPB) guided by ultrasound for post-operative pain and the need for rescue analgesia following laparoscopic cholecystectomy.
Methods: Eighty patients were included in the study who were scheduled for laparoscopic cholecystectomy with 40 patients in each group. Patients were randomly assigned to one of the two groups who underwent ESPB prior to surgery: Group B (ESPB with 20 ml of 0.25% Bupivacaine) or Group R (ESPB with 20 ml of 0.375% Ropivacaine). Pain assessment was done for 24 h postoperatively. Patients received Tramadol 1 mg/kg intravenously as a rescue analgesic if their Numerical rating scale (NRS) was ≥4.
Results: Group R had lower mean NRS at 1 h, 3 h, 6 h, and 24 h, and Inj tramadol as rescue analgesia was less than in Group B.
Conclusion: Ropivacaine 0.375% provided better pain relief in post-operative period, lesser need for analgesia, lower dose of Tramadol requirement in comparison to Bupivacaine 0.25% in ultrasound-guided Erector spinae block.
Keywords: Ropivacaine, Bupivacaine, Erector spinae plane block, Laparoscopic cholecystectomy
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i4.7026 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Laparoscopic Cholecystectomy (LC) is a non-invasive procedure but one of the most prevalent concerns of patients is experiencing pain in the immediate postoperative period [1, 2]. There is a possibility that patients undergoing LC will feel visceral pain as a result of gallbladder resection, abdominal insufflation, and peritoneal distention and injury [3]. Patients may also experience somatic discomfort that originates from port-entry wounds.
A peri-paravertebral fascial plane block, also known as an ESPB, has been shown to be a useful regional anaesthetic intervention for the purpose of providing analgesia following a variety of surgical procedures. ESPB is both simple to conduct without any complications. Multiple studies [3, 4] have showed that ESPB has an analgesic impact on the pain that patients experience after Cholecystectomy. Even though there are an increasing number of studies concerning ESPB, it is still not apparent what the optimal dose of local anaesthetics should be for ESPB in LC settings.
Bupivacaine and Ropivacaine are part of amide family of local anaesthetics and have long duration of action when administered as local infiltration, peripheral nerve blocks and central neural block. Ropivacaine is less cardiotoxic and neurotoxic potential than Bupivacaine [5] due to its lower lipid solubility as compared to Bupivacaine, which is responsible for its lower penetration into myelinated motor fibres and thus causing lesser motor blockade with greater sensory-motor differentiation [5]. According to a research ultrasound-guided ESPB have found Bupivacaine to be very effective in providing postoperative pain relief [6, 7]. Similarly, other studies carried out in ESPB have found Ropivacaine to be effective in postoperative pain management [8-10].
Our study aims to evaluate the analgesic efficacy of Bupivacaine and Ropivacaine using Ultrasound-guided (USG) ESP block for post-operative pain and need for rescue analgesic dosage after Laparoscopic Cholecystectomy.
MATERIALS AND METHODS
The study was done in 80 patients randomly allocated into two groups i. e Group B and Group R by computer-generated random numbers.
Patients between the age of 18 and 60 y of either gender belonging to American society of Anaesthesiologists physical status I and II undergoing elective cholecystectomy laproscopically were included in the study. Refusal from patient, patients with significant coagulopathies and other contraindication, patients with pre-existing systemic diseases, patient allergic to local anaesthetics, infection of the skin at the injection site, any lesion obscuring sono anatomy, patients on anticoagulants, patients with psychiatric illness were excluded from the study. After obtaining ethical clearance from institutional ethics committee and fulfilling the inclusion criteria, patients were divided into two groups at random using computer-generated random numbers after written informed consent was taken.
Group B-received USG-guided Bilateral ESP block with 20 ml of 0.25% Bupivacaine.
Group R-received USG guided Bilateral ESP block with 20 ml of 0.375% of Ropivacaine.
Procedure
All the patients underwent pre-anaesthetic evaluation. On day night before surgery Tab Alprazolam 0.5 mg was given. All the patients were kept nil orally for 8 h. For all patients in the preoperative room baseline vitals, heart rate, mean arterial pressure, oxygen saturation, electrocardiogram were recorded. Intravenous line was secured. Premedication included Inj. Ondansetron 0.1 mg/kg, Inj. Glycopyrrolate 0.004 mg/kg and Inj. Butorphanol 0.03 mg/kg. was given. Patient was shifted to operation theatre and patient was positioned in sitting with mild flexion of body. T7 vertebra was identified by palpating spinous processes. The block site was painted and draped then 45 10MHz frequency linear ultrasound probe was placed longitudinally at the level of the T7 spinous process 3 cm laterally from the midline, next erector spinae muscle and T7 transverse process were located. Under aseptic precautions Sonoplex needle was positioned in the in-plane technique under ultrasound guidance at a 30-40 degree angle and moved from cranial to caudal direction until the tip touched the transverse process of T7, 20 ml of prefilled “study drug” was injected deeply into the erector spinae muscle after hydro-dissection with 2-3 ml of saline to confirm the proper needle tip location. The same process was done on the contra lateral side. Block was administered under standard monitoring. The patient was then preoxygenated with 100% oxygen for a period of three minutes through Bains circuit and induced with Inj Propofol 2 mg/kg IV. Once the eye reflex was lost inj. Succinylcholine 2 mg/kg was given and passage of fasciculations noted then appropriate size cuffed ET tube was used for intubation. Bilateral air entry was confirmed and fixed accordingly. Anaesthesia was maintained with Inj. Atracurium 0.5 mg/kg, intermittent positive pressure ventilation with 33% Oxygen and 66% Nitrous oxide. Carbon dioxide was used to achieve pneumo-peritoneum with a pressure of 12 mmHg. Laparoscopic ports were removed and CO2 was evacuated at the end of surgery. After extubation, the patients were shifted to the post anesthesia care unit. Numerical Rating Scale was used to assess pain in the postoperative period. Patients in the post operative ward were assessed from 1st h till 24th h after surgery using the NRS for pain evaluation. NRS is scored from 1 to 10 where 1 has no pain, score 5 is moderate pain, score 10 is worst possible pain. When the NRS score is ≥ 4, IV Tramadol (75 mg) was given as rescue Analgesia.
Sample size formula
n=4pq/d2
n=4*70*30/20% of 70
n=40 in the minimum sample size for each group.
Where, n= sample size,
p=Prevalence,
q=Non-Prevalence,
d=error
Sample size was calculated taking into account of incidence and prevalence of the hospital record where the study was done. On an average the incidence was 7% per year and from the past 10 y (as per records) the prevalence is 70% (prevalence=incidence*duration).
Statistical analysis
Data was collected using a proforma format. IBM USA's SPSS 26.0 version was used to analyze the data after it was entered into an MS Excel sheet. Proportions were used to represent qualitative data. The mean and standard deviation were used to express quantitative data. Association between two qualitative variables was seen by using Chi square. To determine whether the mean difference between groups is significant, the unpaired t test was used to compare the means and SD of the two groups. Each variable's descriptive statistics was presented using the mean, standard deviation, and standard error of mean. Statistical significance was defined as a p value<0.05, while high significance was defined as a p value<0.001.
RESULTS
Eighty patients were included in the study. The aim of our study is to compare the effect of ropivacaine with bupivacaine in laparoscopic cholecystectomy.
Demographic parameters were noted with respect to mean age, gender, ASA grading, BMI and duration of surgery in both the groups and there was no statistically significant difference between the groups (table 1)
Table 1: Demographic data
| Data | Group-B n=40 | Group-R n=40 | p value |
| Age (Years) | 38.85±9.4 | 38.63±8.25 | 0.91 |
| Gender (Male/Female) | 11/29 | 10/30 | 0.799 |
| ASA Grading-I/II | 30/10 | 24/11 | 0.152 |
| BMI (kg/m2) | 24.28±1.04 | 24.11±0.86 | 0.449 |
| Duration of surgery (min) | 50.1±3.16 | 51.25±3.48 | 0.123 |
Data is represented as mean±SD(standard deviation) or in numbers, ASA (American society of Anesthesiologists), BMI-Body mass index, p value<0.05 is statistically significant
In our study, we have taken numerical rating scale (NRS) to assess the pain after Laparoscopic Cholecystectomy. NRS is 0 and 10 scale where 0 is no pain and 10 is worst pain, in our study we have taken NRS to describe the intensity of postoperative pain verbally.
The mean NRS score at 1 h, 3 h, 6 h and 24 h was statistically significantly lower in Group R compared to group B, p-value of<0.001 (table 2).
In our study it was observed that all patients in the Bupivacaine group needed rescue analgesia in post-operative period. Rescue analgesia in our study was given when patient complained of pain when NRS was ≥ 4 and Inj Tramadol 1 mg/kg IV infusion was given. The mean dose in group R was statistically significantly lower than in group B (table 3).
There are several complications noted with various anaesthetic agents, and this could affect the post-operative comfort of the patient. In our study we observed significantly higher incidence of vomiting with Bupivacaine than with Ropivacaine (fig. 1).
Table 2: Mean numerical rating scale
| NRS (at intervals) | Group B n= 40 | Group R n=40 | p-value |
| 1 h | 2.4±0.3 | 1.8±0.32 | <0.001 |
| 3 h | 2.4±0.3 | 2.03±0.3 | 0.007 |
| 6 h | 2.8±0.59 | 2.18±0.61 | 0.019 |
| 12 h | 3.53±0.49 | 3.4±0.51 | 0.572 |
| 24 h | 3.43±0.38 | 2.55±0.42 | <0.001 |
Data is represented by mean ±SD. p<0.01 is statistically significant, the mean NRS at 12th h was similar in both the groups, Group B and group R.
Table 3: Time taken and dose of first rescue analgesia
| Time | Group B n= 40 | Group R n=40 | p-value |
| First analgesic time (hours) | 12.18±6.69 | 18.48±7.18 | <0.01 |
| Analgesic dose consumption within 24h (mg) | 78.1±17.17 | 52.3±12.45 | 0.003 |
Data is represented by mean ±SD. p<0.01 is statistically significant
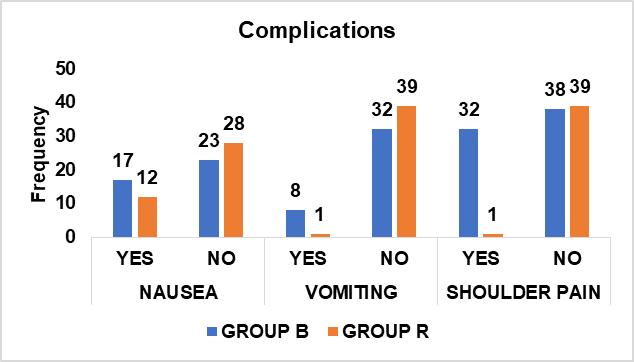
Fig. 1: Bar diagram showing adverse effects
The mean PACU duration and the length of hospitalization was comparable and was not significant among the two groups.
DISCUSSION
The provision of effective postoperative analgesia has a number of advantages, including the enhancement of surgical outcomes, the reduction of postoperative stress response, morbidity, and the length of postoperative hospital stays. Strategies to lessen the severity of adverse effects should be incorporated for post-operative analgesia. When multimodal analgesia is used, which includes peripheral nerve blocks, the use of other analgesics is reduced thus reducing their side effects. Opioids can cause nausea, vomiting, and itching, and nonsteroidal anti-inflammatory drugs (NSAIDS) can have an impact on the healing of wounds, the hepatic system, and the renal system. The erector spinae plane block has been demonstrated to be useful in lowering pain scores and minimising the amount of opioid that is consumed during laparoscopic procedures. There are few studies comparing the use of these two anaesthetic agents in USG-guided ESBP for laparoscopic cholecystectomy. Hence, we have compared using similar studies performed in other surgeries. In our study, we noted that the mean age of the Bupivacaine group was 38.85± 9.4 y, while in the Ropivacaine group it was 38.63±8.25 y. In a study by Sreedhar et al., the mean age between the groups was comparable, with an average of 38 y, similar to that of our study. In our study, there was no difference between gender distribution difference among the groups, our results were similar to the study done by Solanki et al. [11]. In our present study, there was no significant difference between the groups in terms of the BMI, Similar findings were noted in the study by Sreedhar et al. [12]. All the patients in both the groups in our study were haemodynamically stable throughout the study period. However, we noted that the haemodyamics were more stable with Ropivacaine: In the present study, the duration of anesthesia was comparable between the groups, with a longer duration of anaesthesia with Ropivacaine, similar findings were noted with other studies [11-13]. We observed that the duration of anesthesia was significantly longer with the Ropivacaine group than with the Bupivacaine group. In a study by Sreedhar et al., similar findings were noted which coincided with our study [12]. The mean tramadol dose in group B was significantly higher than in the Ropivacaine group. In the present study, we observed Bupivacaine group needed significantly more number of rescue analgesia in comparison with ropivacaine group. The occurrence of complications is uncommon due to the considerable distance between the injection site and the pleura, major blood arteries, and the spinal cord. The main drawbacks of ESPB include infection at the site of needle insertion, puncture of blood vessels, puncture of the pleura, pneumothorax, and unsuccessful block.
Local anesthetic (LA) solution is administered beneath the erector spinae muscle and superficial to transverse process in ESP Block. Then the drug spreads everywhere. It permeates to paravertebral area and blocks both somatic and visceral sensations. The LA targets the spinal neurons' ventral and dorsal rami as well as rami communicantes [14]. During LC, this block has been effective as a component of multimodal analgesia. Using ultrasound to deposit local anaesthetics deep to the three columns of the erector spinae group of muscles (iliocostalis, longissimus, and spinalis) is advocated for conducting an ESP block. Studies have found that Bilateral ultrasound-guided ESPB resulted in effective analgesia and a reduction in analgesic needs during the first 12 h in patients, where both somatic and visceral pain are present [14].
A research conducted by Ruchi Verma et al. [15] involving 85 adults who were posted for elective LC were randomized to receive bilateral ESPB at the T7 level with either 20 ml of 0. 375% ropivacaine or 20 ml of normal saline. Visual analog scale (VAS) was used to record postoperative static and dynamic scores. Fentanyl requirement intraoperatively, diclofenac use in postoperative period, time to ambulation following surgery, and presence of postoperative pain were noted and they concluded static and dynamic VAS scores, intraoperative fentanyl requirement and number of patients requiring diclofenac postoperatively were significantly lower in ESPB group, while number of patients ambulating by 4 h were higher in ESPB group. Patients suffering from pain till 7 days were lower in ESPB group. Similar findings were observed by study conducted by Basak Altiparmak et al. [16].
In a study done by Nachiket A. Solanki et al. [11] 60 patients were selected, aged 18 to 60, who were posted for laparoscopic cholecystectomy and were allocated into two groups: Group B (bupivacaine) and Group R (ropivacaine). At the level of the thoracic ninth vertebrae, a bilateral erector spinae block was carried out prior to the onset of general anesthesia. This investigation revealed that group R (ropivacaine) had a lower VAS score than group B (bupivacaine). Compared to group B, group R had analgesia for a longer time compared to group B. Group R performed better in terms of post-operative VAS score and analgesia.
All the above study findings and results were coinciding with our present study, in the present study, we found that there was lesser post-operative pain, lesser need for analgesia, lower dose of tramadol consumption, quick ambulation and lower complications in Group R patients compared to patients in Group B.
Limitations of our study: Sample size was calculated taking into account of incidence and prevalence of the hospital record where the study was done with limited population. The study was done by giving GA were effect of onset of block could not be assessed. Pain sensitivity and tactile sensation were not considered. Larger sample size will eliminate the bias.
CONCLUSION
Ropivacaine 0.375% provided better pain relef in post-operative period, lesser need for analgesia, lower dose of Tramadol requirement in comparison to Bupivacaine 0.25% in ultrasound guided Erector spinae block.
ACKNOWLEDGEMENT
The authors are grateful for the cooperation of the patients for the study.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
CONFLICT OF INTERESTS
Declared none
REFERENCES
Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997;79(3):369-78. doi: 10.1093/bja/79.3.369, PMID 9389858.
Gerbershagen HJ, Aduckathil S, Van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934-44. doi: 10.1097/ALN.0b013e31828866b3, PMID 23392233.
Shin HJ, Oh AY, Baik JS, Kim JH, Han SH, Hwang JW. Ultrasound guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: a randomized controlled observer-blinded study. Minerva Anestesiol. 2014;80(2):185-93. PMID 24193176.
Aydin G, Aydin O. The efficacy of ultrasound-guided paravertebral block in laparoscopic cholecystectomy. Medicina (Kaunas). 2018;54(5):75. doi: 10.3390/medicina54050075, PMID 30360531.
Altıparmak B, Korkmaz Toker M, Uysal AI, Kusuu Y, Gumus Demirbilek S. Ultrasound guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: randomized controlled trial. J Clin Anesth. 2019 Nov;57:31-6. doi: 10.1016/j.jclinane.2019.03.012, PMID 30851501.
El Ghamry MR, Elgebaly AS, Anwar AG, Shaddad MN. Ultrasound-guided erector spinae plane block for acute pain management in patients undergoing posterior lumbar interbody fusion under general anaesthesia. South Afr J Anaesth Analg. 2019;25(6):26-31. doi: 10.36303/SAJAA.2019.25.6.A4.
Singh S, Chaudhary NK. Bilateral ultrasound-guided erector spinae plane block for postoperative pain management in lumbar spine surgery: a case series. J Neurosurg Anesthesiol. 2019;31(3):354. doi: 10.1097/ANA.0000000000000518, PMID 29965831.
Gonzalez S, Basora MM, Tio M, Camacho A, Fuster S, Blanch X. L4 erector spinal plane block after lumbar spine arthrodesi: a case series. Rev Esp Anestesiol Reanim. 2019 Dec;66(10):537-42. doi: 10.1016/j.redar.2019.05.004.
Jin Y, Zhao S, Cai J, Sun Y, Blessing M, Hu S. Efficacy of ultrasound guided erector spinae plane block for perioperative pain control and short-term outcomes in lumbar laminoplasty. BMJ Yale. 2020;19(7):45. doi: 10.1101/2020.01.30.20019745.
Yao Y, Li H, He Q, Chen T, Wang Y, Zheng X. Efficacy of ultrasound guided erector spinae plane block on postoperative quality of recovery and analgesia after modified radical mastectomy: randomized controlled trial. Reg Anesth Pain Med. 2019:rapm-2019-100983. doi: 10.1136/rapm-2019-100983, PMID 31678959.
Solanki NA, Korat RR, Shah DV, Patel SK. Evaluation of analgesic efficacy of bupivacaine and ropivacaine given through landmark guided erector spinae plane block for post-operative pain relief in patients undergoing laparoscopic cholecystectomy. Natl J Med Res. 2020 Jul-Sep;10(3):144-7.
Sreedhar N, Hemlata MMK, Mehrotra MK, Singh PR, Siddiqui AK, Kohli M. Efficacy of bilateral erector spinae plane block using bupivacaine and ropivacaine for postoperative analgesia following lumbar spine surgeries a randomised clinical study. J Clin Diagn Res. 2021 Sep;15(9):UC19-UC23. doi: 10.7860/JCDR/2021/49463.15397.
Sifaki F, Mantzoros I, Koraki E, Bagntasarian S, Christidis P, Theodoraki K. The effect of ultrasound-guided bilateral erector spinae plane block with and without dexmedetomidine on intraoperative and postoperative pain in laparoscopic cholecystectomies: a randomized controlled double blind prospective trial. Pain Physician. 2022 Oct;25(7):E999-E1008. PMID 36288585.
Schnabel A, Weibel S, Pogatzki Zahn E, Meyer Frießem CH, Oostvogels L. Erector spinae plane block for postoperative pain. Cochrane Database Syst Rev. 2023;10(10):CD013763. doi: 10.1002/14651858.CD013763.pub2, PMID 37811665.
Verma R, Srivastava D, Saxena R, Singh TK, Gupta D, Agarwal A. Ultrasound-guided bilateral erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a randomized controlled trial. Anesth Essays Res. 2020 Apr-Jun;14(2):226-32. doi: 10.4103/aer.AER_41_20, PMID 33487820.
Altıparmak B, Korkmaz Toker M, Uysal AI, Kuscu Y, Gumus Demirbilek S. Ultrasound guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: randomized controlled trial. J Clin Anesth. 2019 Nov;57:31-6. doi: 10.1016/j.jclinane.2019.03.012, PMID 30851501.