
Int J Curr Pharm Res, Vol 17, Issue 3, 29-32Original Article
PERCEPTION OF ONLINE AND OFFLINE LEARNING AMONG MBBS STUDENTS IN A TERTIARY CARE HOSPITAL IN MANIPUR: A CROSS-SECTIONAL STUDY
NEERAJ KUMAR SHARMA MANOHAR1*, THANGJAM RUBEE2, NGAMBA AKHAM3, OINAM JOYCHANDRA SINGH4
1,4Department of Pharmacology, Shija Academy of Health Sciences, Manipur, India. 2Department of Microbiology, Shija Academy of Health Sciences, Manipur, India. 3Department of Community Medicine, Shija Academy of Health Sciences, Manipur, India
*Corresponding author: Neeraj Kumar Sharma Manohar; *Email: neeraj_eigya@yahoo.in
Received: 22 Jan 2025, Revised and Accepted: 11 Mar 2025
ABSTRACT
Objective: The objectives of the present study were to evaluate the responses of undergraduate medical students on online and offline learning methods and to find associations between selected variables.
Methods: A cross-sectional questionnaire-based study was conducted at Shija Academy of Health Sciences, Imphal-west, Manipur, with 284 Phase-2 and Phase-3 Undergraduate MBBS students. A validated, self-administered questionnaire consisting of 20 Likert-scale questions was distributed, and 227 complete responses were analyzed. Data analysis was performed using SPSS v25, employing chi-square tests for associations.
Results: The majority of students preferred offline learning over online classes. Key findings include:
Over 70% found offline classes easier for grasping concepts, regaining attention, and facilitating engagement and guidance.
Students valued online classes for their flexibility, convenience during illness, and ability to overcome disturbances (e. g., curfews or blockades).
However, 72.2% believed online classes could not replace offline learning, particularly for technical medical education requiring hands-on skills.
Statistically significant associations (p<0.05) were observed between key variables, including preferences for offline interaction, learning efficiency, and the convenience of online education.
Conclusion: The study underscores the complementary role of online method advocating for a hybrid approach to optimize competency-based medical education (CBME) in Manipur outcomes. Moreover, offline courses are more suitable more technical courses involving manual and practical training.
Keywords: Online, Offline, Interactive, Engagement, Flexibility, Accessibility, Hybrid, CBME
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i3.55047 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
The traditional theory teaching method has always involved a classroom setting with a teacher delivering face-to-face lectures with the students giving attention, jotting down notes, asking questions and also receiving answers to the questions asked [1].
However, with the impact of COVID-19 pandemic, e-learning or online teaching has slowly paved its way into mainstream educational modus operandi. Accordingly, educational Institutes have made a shift from offline to online teaching and learning media through Google meet, Microsoft teams, etc [2].
The 1st online course was given in the year 1981 with the first online program prepared by the Western Behaviour Sciences Institute the following year [3].
With numerous uncertainties at hand, starting from natural calamities to blockades and bandhs alike, several teachers have now switched over and somewhat adapted to online teaching mode [4].
Since the pandemic, health science students have also started leaning towards online education in respective disciplines [5, 6].
Teaching-learning process in the field of health viz., medicine, dentistry, nursing, physiotherapy and other allied departments, vary in this curriculum. It involves both the theoretical and practical aspects in the lecture halls, clinical wards and clinical laboratories [7, 8].
In India, a new curriculum has been introduced under the name CBME which dictates competency-based medical education since 2019. This was developed by the Medical Council of India with the Curriculum Implementation Support Program (CISP) [9, 10].
The key players of CISP are the faculty of medical education department of regional and nodal centres to which all colleges of India are attached. The novel aspects of CBME include Foundation course, early clinical exposure, attitude, ethics and communication (AETCOM), integrated teaching and skill training [10-13].
Online learning has multiple benefits like flexibility, availability of plenty of options, cost-effectiveness, comfortable as per environment, etc. However, no pedagogical approach can replace the traditional face-to-face learning. Classroom teaching learning enhances students’ critical thinking skills and provides an opportunity for students to engage in the live discussions [14, 15].
As such, it is very important to evaluate the perception of the students on how online and offline modes of study effect their learning curriculum. Hence, the present study is conducted to obtain the views and opinions of undergraduate medical students in regards to online and offline learning in the currently undergoing CBME curriculum for better medical education.
MATERIALS AND METHODS
Study design: It was a questionnaire based cross-sectional study.
Study setting: It was conducted inside the lecture hall of Shija Academy of Health Sciences (SAHS).
Study area: Imphal-West, Manipur.
Study duration: 22/10/2024-28/10/2024.
Study population: All phase-2 and phase-3 part-1 Undergraduate MBBS students of SAHS.
Inclusion criteria: Those who consented
Exclusion criteria: Those who were absent on the day of distributing the questionnaire
Sample size: 284 undergraduate medical students of phase-2 and phase-3 part-1 MBBS students.
Sampling method: Universal sampling
Study tool: A validated self-administered questionnaire formed referring to previous investigators was used for the study [5, 7, 8]. It included 20 likert type questions answered on a 5-point scale (1= Strongly agree, 5= strongly disagree).
Study variables: Socio-demographic information of the Undergraduate medical students such as age, gender, etc.
Data collection Procedure: Participants were briefed regarding the responses to be filled in the questionnaire during working hours from 9 am to 10 am. After obtaining verbal consent, a total of 284 questionnaires was distributed to the undergraduate medical students of phase-2 and phase-3 part-1 MBBS. Each filled questionnaire was collected back on the same day and kept in the Dept. of Pharmacology, SAHS.
Statistical analysis: the collected data was first entered in MS Excel and checked for data consistency and corrections. Line diagram and chi-square test was utilized for data analysis with SPSS v25 (IBM, ARMONK, NY).
Ethical considerations: Ethical clearance dated 25/04/2024 vide order no. IEC/SAHS/APR/24-002 was sought from the Institutional Ethical Committee, SAHS. No personal identifiers were used during the data collection. Privacy and confidentiality maintained and the data was kept under lock and key in the Dept. Of Pharmacology, SAHS.
Funding: It was self-funded.
RESULTS
Out of the 284 questionnaires distributed, 227 were found to be complete in the total responses and hence, the data was analysed on the completed 227 questionnaires with a chi-square test using SPSS v25 (IBM, ARMONK, NY).
Out of the 227 students, males attributed to 83 (36.5%), while female accounted for 144 (63.5%) of the responses. All of them had online learning experience in the past.
The participants responded to each of the questionnaire using a 5-point Likert Scale ranging from strongly agree to strongly disagree.
Table 1: Cumulative response by the participants
| Responses | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| Q1. It is much easier to grasp the information when the speaker is directly in front of you in an offline class. | 74 | 112 | 30 | 8 | 3 |
| Q2. It is not distracting when you are surrounded by your colleagues also attending the offline class. | 39 | 141 | 29 | 12 | 6 |
| Q3. It is easier to regain attention by looking at the teacher in case one loses concentration in the offline class. | 48 | 120 | 48 | 8 | 3 |
| Q4. Offline class is less disrupting than online class. | 71 | 94 | 45 | 3 | 14 |
| Q5. Offline class engages students to learn more compared to online class. | 95 | 74 | 51 | 0 | 7 |
| Q6. Offline teaching is more reliable than online teaching. | 80 | 85 | 55 | 4 | 3 |
| Q7. Offline class is more well-guided compared to online class. | 80 | 83 | 49 | 12 | 3 |
| Q8. Offline classes give more chances of interaction amongst the students. | 119 | 101 | 4 | 0 | 3 |
| Q9. Hints of important topics for the examinations are better given in offline classes. | 83 | 65 | 64 | 12 | 3 |
| Q10. Teachers in offline classes are more engaging as compared to online classes. | 83 | 65 | 64 | 12 | 3 |
| Q11. Online classes are extremely useful in cases of short-term illness. | 54 | 128 | 45 | 0 | 0 |
| Q12. Online classes are helpful in case of unintended disturbances viz., curfew, bandhs, blockades. | 89 | 107 | 31 | 0 | 0 |
| Q13. Online classes save the time of students as they can attend at home. | 62 | 92 | 54 | 15 | 4 |
| Q14. Online classes save the money of students as they do not need to travel. | 43 | 78 | 86 | 16 | 4 |
| Q15. Online classes cannot replace offline classes. | 25 | 0 | 38 | 102 | 62 |
| Q16. Online classes are more interesting as there are animations, videos, etc. | 24 | 50 | 118 | 28 | 7 |
| Q17. Online classes are not good for technical courses including medical stream. | 10 | 14 | 82 | 65 | 56 |
| Q18. Online classes are not convenient if there is interruption of internet. | 14 | 55 | 112 | 35 | 11 |
| Q19. Online classes allow us to learn at our own pace. | 36 | 81 | 81 | 16 | 13 |
| Q20. Online classes are hassle-free. | 29 | 62 | 115 | 11 | 10 |
Table 2: Demographic profile of the sample
| Age | Frequency | Percentage |
| 18 | 8 | 3.5% |
| 19 | 26 | 11.4% |
| 20 | 58 | 25.5% |
| 21 | 70 | 30.7% |
| 22 | 30 | 13.2% |
| 23 | 20 | 8.8% |
| 24 | 10 | 4.4% |
| 25 | 4 | 1.7% |
| 26 | 1 | 0.4% |
| Total | 227(Males=83, Females=144) |
On testing the Association between “It is much easier to grasp the information when the speaker is directly in front of you in an offline class” and “It is easier to regain attention by looking at the teacher in case one loses concentration in the offline class”, the p-value was 0.000 which was statistically significant.
Then, on analysis, the association between “Offline class engages students to learn more compared to online class” and “Offline class is more well guided compared to online class”, the p-value was 0.001, which was significant.
Further, testing the association between “Online classes are extremely useful in cases of short-term illness” and “Online classes are helpful in case of unintended disturbances viz., curfew, bandhs, blockades” p-value was 0.001, which was again statistically significant.
Again, association on “Online classes save the time of students as they can attend at home” And “Online classes save the money of students as they do not need to travel”, the p-value was 0.000, which was statistically significant.
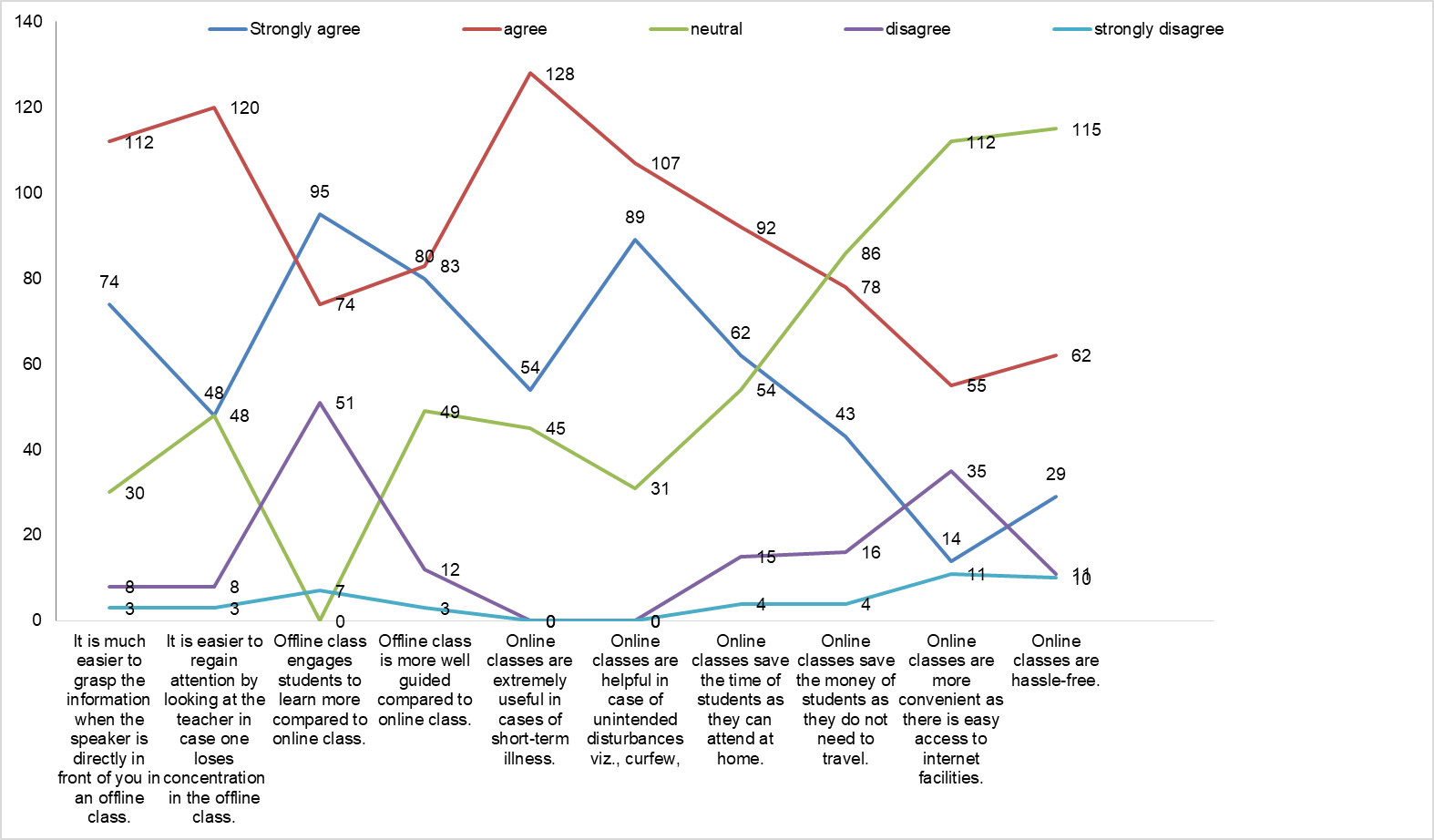
Fig. 1: Line diagram depicting the responses of the participants on selected variables
Finally, an association between “Online classes are more convenient as there is easy access to internet facilities” and “Online classes are hassle-free”, the p-value was 0.001, which too was significant.
DISCUSSION
The present study sought to evaluate the perception of students on offline and online mode of learning. Medical schools will now need to be prepared to train the next generation of digital learners using virtual learning environments. This does not mean that traditional classroom teaching will become obsolete. Both methods can be employed in a hybrid manner to make the process of learning more efficient and effective [16]. In this study, we focused mainly on undergraduate students, as they are the prime stakeholders within the health care system with the success of any teaching model depending on their experiences and perceptions.
According to the feedback and questionnaire survey of students, it was reflected that the students preferred more of offline classes than the online classes since majority of the students i. e., more than 70% of them perceived that offline classes are easier to grasp and regain attention, less disrupting, well guided and engaged the students more than online classes which resonates well with another study [17] in which more than 50% of their students showed a preference for traditional learning. Also, in another survey, it was shown that the majority of the students did not find the online teaching sessions to be stimulating, engaging or enjoyable [18]. Only 17.6% of the students felt strongly that online teaching was stimulating, 19.6% of the students felt strongly that they could engage themselves in these online learning methods.
An interpretation of the findings obtained in this study also indicated that online classes are more convenient to some of the students as they can learn in their own pace which was supported by findings in other settings [19, 20]. However, 96.9% of the students felt that the offline classes provide the better platform for student teacher interactions and interactions among peers. These findings supported previous research suggesting that interactions among peers and teachers with the learners are difficult in online classes in other studies on perception of students regarding online learning during the COVID pandemic [21, 22].
Furthermore, in another study, online classes faced technical problems and have made students feel frustrated [23]. Similarly, more than 80% of the students in this study also agreed that online classes are very useful in cases of sickness unintended disturbances such as curfew. In addition, more than 50% 0f them felt that online classes save time and money of students as they can attend from home and do not need to travel having said that majority of the students However, 72.2%, also felt that online classes cannot replace the offline classes as most of them agreed that online classes are not good for technical courses including medical stream since one cannot learn in online classes the clinical skills which is also a similar interpretation obtained before [24], suggesting that online learning was less effective for practical or lab-based courses than it was for theory-based courses.
LIMITATIONS
The study was conducted at one institution. The data obtained and conclusions drawn were specific to this environment. However, similar studies could be done in other hospitals in order to get a more complete picture of online and offline learning in Manipur.
CONCLUSION
Traditional classes or the chalk and-board method of learning is still the major teaching method everywhere around the world. The same was dictated as observed in the findings of this current study. The changing pace of technology is slowly seeping online method of education in every nook and corner of modern education. This accounts for multiple changes in the teachers to adapt to the new ways of learning. No doubt a robust internet facility will be a must to ensure hassle-free access to the online methods in the coming future for all educational institutions both in the rural and peripheral locations. This is also important in regards to medical education in India as we are following the Competency-based Medical Education (CBME), which involves computer-aided learning sessions utilising internet facility. The role of the educators in the future would be to ensure that both the traditional offline and online teaching is imparted as per the requirement of that point of time.
ACKNOWLEDGEMENT
The authors would like to thank the Director and Dean of SAHS, the staff of Dept. of Pharmacology, SAHS and all the participants involved for their co-operation and time in completing this survey.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICT OF INTERESTS
Declared none
REFERENCE
O Malley J, MC Craw H. Students perceptions of distance learning online learning and the traditional classroom. Online J Dist Learn Admin. 1999;2:1-10.
Saiyad S, Virk A, Mahajan R, Singh T. Online teaching in medical training: establishing good online teaching practices from cumulative experiences. Int J Appl Basic Med Res. 2020;10(3):149-55. doi: 10.4103/ijabmr.IJABMR_358_20, PMID 33088735.
Harasim L. Shift happens: online education as a new paradigm in learning. The Internet and Higher Education. 2000;3(1-2):41-61. doi: 10.1016/S1096-7516(00)00032-4.
Dhawan S. Online learning: a panacea in the time of COVID-19 crisis. J Educ Technol Syst. 2020;49(1):5-22. doi: 10.1177/0047239520934018.
Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378. doi: 10.1136/bmjopen-2020-042378, PMID 33154063.
Wang C, Xie A, Wang W, WU H. Association between medical students prior experiences and perceptions of formal online education developed in response to COVID-19: a cross sectional study in China. BMJ Open. 2020;10(10):e041886. doi: 10.1136/bmjopen-2020-041886, PMID 33122327.
Michel A, Ryan N, Mattheus D, Knopf A, Abuelezam NN, Stamp K. Undergraduate nursing students perceptions on nursing education during the 2020 COVID-19 pandemic: a national sample. Nurs Outlook. 2021;69(5):903-12. doi: 10.1016/j.outlook.2021.05.004, PMID 34183191.
Rossettini G, Geri T, Turolla A, Viceconti A, Scuma C, Mirandola M. Online teaching in physiotherapy education during COVID-19 pandemic in Italy: a retrospective case control study on students satisfaction and performance. BMC Med Educ. 2021;21(1):456. doi: 10.1186/s12909-021-02896-1, PMID 34455979.
Medical Education Unit Revised Programme of Basic Course workshop. Available from: https://www.cmch-vellore.edu/sites/med/RBCW.
Medical Council of India. Curriculum Implementation Support Program (CISPI): first year report. Available from: www.nmc.orghttps://www.in/wp-content/uploads/2020/09/CISP-I-First-year-Report-2019_11.09.2020-2.pdf.
Medical Council of India. Competency-based undergraduate curriculum for the indian medical graduate volume 3. Available from: https://www.nmc.org.in/wp-content/uploads/2020/01/UG-Curriculum-Vol-III.pdf.
Medical Council of India. Competency-based undergraduate curriculum for the indian medical graduate-volume 2. Available from: https://www.nmc.org.in/wp-content/uploads/2020/01/UG-Curriculum-Vol-II.pdf.
Medical Council of India. Competency-based undergraduate curriculum for the indian medical graduate-volume 1. Available from: https://www.nmc.org.in/wp-content/uploads/2020/01/UG-Curriculum-Vol-I.pdf.
Maheshwari K, Ladha N, Khapre M, Deol R. Perception of online learning among health sciences students a mixed methods study. J Educ Health Promot. 2022 Sep 28;11:286. doi: 10.4103/jehp.jehp_364_22, PMID 36438998.
Reeves S, Fletcher S, MC Loughlin C, Yim A, Patel KD. Interprofessional online learning for primary healthcare: findings from a scoping review. BMJ Open. 2017;7(8):e016872. doi: 10.1136/bmjopen-2017-016872, PMID 28780560.
Kumari A, Rani S, Bara MP. A study on the perception of medical students using online teaching during COVID-19 pandemic. J Fam Med Prim Care. 2022;11(6):2552-6. doi: 10.4103/jfmpc.jfmpc_2074_21, PMID 36119297.
Saurabh MK, Patel T, Bhabhor P, Patel P, Kumar S. Students perception on online teaching and learning during COVID-19 pandemic in medical education. Maedica (Bucur). 2021;16(3):439-44. doi: 10.26574/maedica.2021.16.3.439, PMID 34925600.
Rao P, Panja S, Chattopadhyay M, Biswas J, Dhali A, Dhali GK. Perception of online learning among undergraduate medical students of Eastern India: a cross-sectional study. Cureus. 2022 Dec 16;14(12):e32580.
Dost S, Hossain A, Shehab M, Abdelwahed A, Al Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378. doi: 10.1136/bmjopen-2020-042378, PMID 33154063.
Karaman S. Nurses perceptions of online continuing education. BMC Med Educ. 2011;11:86. doi: 10.1186/1472-6920-11-86, PMID 22013974.
Ansar F, Ali W, Khattak A, Naveed H, Zeb S. Undergraduate students perception and satisfaction regarding online learning system amidst COVID-19 pandemic in Pakistan. J Ayub Med Coll Abbottabad. 2020;32 Suppl (4):S644-50. PMID 33754524.
Abbasi MS, Ahmed N, Sajjad B, Alshahrani A, Saeed S, Sarfaraz S. E-learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work. 2020;67(3):549-56. doi: 10.3233/WOR-203308, PMID 33185620.
Fernandez Aleman JL, Carrillo DE Gea JM, Rodriguez Mondejar JJ. Effects of competitive computer assisted learning versus conventional teaching methods on the acquisition and retention of knowledge in medical surgical nursing students. Nurse Educ Today. 2011;31(8):866-71. doi: 10.1016/j.nedt.2010.12.026, PMID 21255880.
Khan MY, Raza SA, Sibtain M. Online learning and motivational strategies in the backdrop of COVID-19: an EFL perspective on teachers and students perceptions at tertiary level in Pakistan. OJS. 2021;4(1):135-47. doi: 10.36902/sjesr-vol4-iss1-2021(135-147).