
Int J Curr Pharm Res, Vol 17, Issue 4, 117-119Original Article
COMPARATIVE STUDY IN UNDERLAY MYRINGOPLASTY WITH TEMPORALIS FASCIA GRAFT ON EITHER SIDE OF HANDLE OF MALLEUS IN TERMS OF GRAFT UPTAKE AND HEARING OUTCOME
MANASAVEENA P., RAGHU CHANAKYA K. S.*, YUGANDHAR G., UDAY SRIKAR V. S.
Department of Oto Rhino Laryngology, GITAM Institute of Medical Sciences and Research, GITAM Deemed to be University, Visakhapatnam-530045, Andhra Pradesh, India
*Corresponding author: Raghu Chanakya K. S.; *Email: drraghuchanakyaent@gmail.com
Received: 17 Apr 2025, Revised and Accepted: 06 Jun 2025
ABSTRACT
Objective: The objective of the study was to compare the two techniques of underlay myringoplasty with graft placed lateral to the handle of malleus.
Methods: 50 patients of chronic otitis media, mucosal, inactive, aged between 18-55 years who presented to ENT OPD with small, medium, large and subtotal perforations having mild to moderate conductive hearing loss were included in the study. After taking informed consent, patients were randomly divided into 2 groups containing 25 patients each. In group A, graft was placed lateral to the handle of malleus and medial to the annulus (underlay technique), while in group B, graft was placed medial to the handle of malleus and medial to the annulus (over underlay technique). Both groups were reviewed after 6 mo. Pre-operative and post-operative air bone gap were compared. Surgery was considered successful based on post-operative graft uptake, hearing improvement and maintenance of middle ear space.
Results: In both groups, 1 participant (4.0%) had not taken the graft, while 24 participants (96.0%) had taken the graft successfully. The total number of participants in each group was 25. The p-value for this comparison is 1.000, indicating no statistically significant difference in the graft position outcomes between the two groups.
Conclusion: Placement of temporalis fascia graft, medial or lateral to the handle of malleus are equally effective in terms of complete graft uptake and post operative hearing gain after 6 mo follow up.
Keywords: Myringoplasty, Underlay technique
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i4.7040 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Chronic otitis media is defined as long standing inflammation of the middle ear and mastoid mucoperiosteum, with recurrent discharge through a chronic perforation of the tympanic membrane. There are two types of Chronic otitis media: Tubo-tympanic (mucosal) and attico antral (squamous). In tubo-tympanic or mucosal type of COM, there is permanent perforation of pars tensa with an inflammed middle ear mucosa which produces mucopus that may discharge. The management of COM include medical management with antibiotics, surgery and hearing aid. Myringoplasty is the surgery performed in majority of the cases and is the definitive one in the management of COM by closing the perforation of tympanic membrane. From the 17th to the 19th century, many efforts were made to repair perforations in the tympanic membrane using prosthetic materials like paper patches and cauterizing agents. The first surgical attempt was made by Banzer in 1640 using a pig's bladder [1]. Berthold introduced the term Myringoplasty [2, 3] in 1878. Wullstein announced [2, 3] a technique using split-thickness skin graftsin 1952. Heerman utilized temporalis fasica in 1958. Shea pioneered underlay tympanoplasty [1]. We are comparing the two techniques of underlay myringoplasty in our study. “One technique involves positioning the graft next to the handle of the malleus [3, 4] while the other method involves positioning the graft on the opposite side of the handle [3]. We are comparing these two approaches in terms of graft uptake and hearing outcome. Storrs is the first person to use temporalis fascia as an underlay graft in 1961. The objectives of the study are to evaluate the graft uptake rate of the two techniques and to evaluate the hearing outcome of the two techniques.
MATERIALS AND METHODS
A prospective study was carried out from 29th September 2022 to 30th April 2024, which included 50 patients who presented to the OPD of Department of ENT at GIMSR, Visakhapatnam, Andhra Pradesh. Those fulfilling the inclusion and exclusion criteria were selected for the study.
Inclusion criteria
Inclusion criteria includepatients age group between 18-55years, patients having small, medium, large and subtotal perforations, those with COM, mucosal type and with dry ear for at least 6 w before operation and patients with mild and moderate conductive hearing loss.
Exclusion criteria
Exclusion criteria include patients with age<18and>55years, with COM, those actively discharging ear and those patients with sensorineural hearing loss.
After obtaining written consent, patients were divided into two groups. We did underlay technique for Group and for Group B. Intra-operatively, temporalis fascia was placed lateral to the handle of malleus in group A. In group B, temporalis fascia was placed medial to the handle of malleus.
RESULTS
The study sample consisting of sixty patients were divided into two separate groups. Each group contained 25 patients of either sex. In Group A, graft was placed by underlay technique lateral to the handle of malleus and in Group B, graft was placed medial to the handle of malleus by underlay technique. Group A consisted of 25 patients, out of which, 13 were females and 12 were males. In case of group B, 9 were females and 16 were males. All patients in group A were aged between 18-55 y and in case of Group B, it was between 18-51 y. Ear discharge and hearing loss were the most common complaints of the patients. Tympanic membrane perforations were classified into four types based on the surface area of pars tensa of the tympanic membrane deficient, namely small (<25%), medium (25-50%), large (50-75%) and subtotal (>75%). Most of the patients had a large central perforation or subtotal perforation. In Group A, thirteen patients (43.3%) suffered from left ear chronic otitis media, 21 patients had unilateral chronic otitis media and 4 patients had bilateral chronic otitis media. In case of Group B, 20 patients suffered from unilateral chronic mucosal disease, 5 patients suffered from bilateral chronic mucosal infection of ear. Pre-operative and post-operative decibels of hearing loss were assessed. Hearing loss was classified into mild (25-40 dB) and moderate (41-55 dB) based on the pure tone audiometry values mean pre-operative value of hearing loss was 35.56±6.82 dB in Group A, whereas in Group B it was 37.04±9.51 dB (table 4). Post-operative hearing improvement (A-B gap) in both groups was assessed after 6 mo. mean A-B gap improvement in group A is 17.56 with a standard deviation (SD) of 5.895, a median of 18.00, and a range from 10 to 40. For the medial to the malleus group, the mean AB gap is 18.84 with an SD of 5.226, a median of 18.00, and a range from 15 to 42. The p-value for the comparison is 0.421, indicating no significant difference statistically in the post-operative 6-month AB gap between the two groups.
Table 1: Graft taken with respect to site of perforation
| Site of perforation | Graft taken in group A (%) | Graft taken in group B (%) |
| Anterior | 100 | 100 |
| Inferior | 100 | 100 |
| Posterior | 100 | 100 |
| Sub total | 96 | 96 |
Table 2: Hearing outcome with respect to site of perforation
| Site of perforation | Hearing outcome in group A (%) | Hearing outcome in group B (%) |
| Anterior | 100 | 100 |
| Inferior | 100 | 100 |
| Posterior | 100 | 100 |
| Sub total | 96 | 96 |

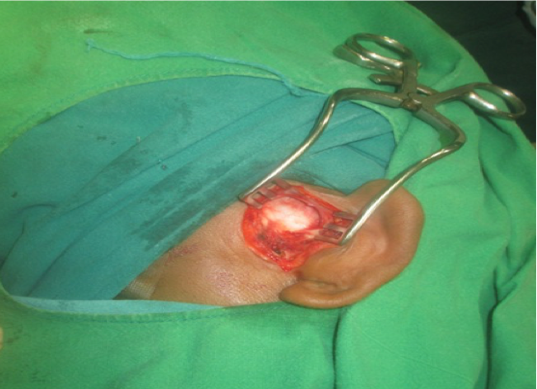
Fig. 1: Showing temporalis fascia graft harvesting
DISCUSSION
Repairing ear drum perforations located anterior to the handle of malleus can be challenging due to a lack of anterior support for the graft in traditional underlay techniques, often resulting in graft failure [4-6]. To address this issue, Sheehy and Anderson introduced the Onlay myringoplasty technique in 1980, which was later followed by various modifications to the classical underlay method. Yung et al. [7] have documented graft take rate of 80% in 51 my ringoplasties in young and older children; true success was found only in two thirds of these cases. Mangia et al. reported success rate of 84% in terms of perforation closure. We found both the techniques are equally effective in terms of complete graft take up and post-operative hearing gain after 3 mo follow up [8]. This research is focused on comparing the results of two modifications of underlay myringoplasty techniques in two different groups of patients, one with the graft placed on the lateral side and the other on the medial side of the handle of the malleus. On the whole, group A has a success rate of 96%, while group B has a success rate of 96%. There is no significant statistical variance between the two groups. Specifically, in terms of anterior perforations, all patients in group A showed a graft uptake rate of 100%, whereas in group B, the rate was also 100%. When looking at perforations in posterior quadrant, both group A and group B have a success rate of 100%. For inferior perforations, the success rate in group A and group B was 100%. Lastly, in cases of subtotal perforations, group A and group B have a success rate of 96%.
CONCLUSION
From the present study findings, the authors had concluded that, comparing the results of two modifications of underlay myringoplasty techniques in two different groups of patients, one with the graft placed on the lateral side and the other on the medial side of the handle of the malleus found that, group A has a success rate of 96%, while group B has a success rate of 96%. There is no significant statistical variance between the two groups.
ACKNOWLEDGEMENT
We are thankful to the department of ENT, GITAM institute of medical sciences and research, Visakhapatnam, Andhra Pradesh for their support.
ETHICAL APPROVAL
The study was approved by the Institutional Ethics Committee (IEC-82/2022)
FUNDING
No funding sources
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICT OF INTERESTS
Declared none
REFERENCES
Ray S, Ghosh S, Jana A, Sit S, Basu SK. Comparative study of graft placement between medial and lateral to malleus in tympanoplasty. Bengal J Otolaryngol Head Neck Surg. 2023;30(3):319-22. doi: 10.47210/bjohns.2022.v30i3.897.
Murugendrappa MA, Siddappa PN, Shambulingegowda A, Basavaraj GP. Comparative study of two different myringoplasty techniques in mucosal type of chronic otitis media. J Clin Diagn Res. 2016 Feb;10(2):MC01-3. doi: 10.7860/JCDR/2016/16843.7194, PMID 27042491, PMCID PMC4800556.
Panchal V, Gulia JS, Yadav SS, Hernot S, Kathuria B, Kaintura M. To evaluate and compare the results of over underlay graft technique with conventional underlay myringoplasty. Indian J Otol. 2015;21(4):274-9. doi: 10.4103/0971-7749.164551.
Rastogi S. Modified technique of underlay myringoplasty. JOENTR. 2018;10(5):269-72. doi: 10.15406/joentr.2018.10.00359.
Stage J, Bak Pedersen K. Underlay tympanoplasty with the graft lateral to the malleus handle. Clin Otolaryngol Allied Sci. 1992 Feb;17(1):6-9. doi: 10.1111/j.1365-2273.1992.tb00978.x, PMID 1555321.
Fiorino F, Barbieri F. Over under myringoplasty with umbus anchored graft. J Laryngol Otol. 2008 Aug;122(8):854-7. doi: 10.1017/S0022215108001874, PMID 18353198.
Yung M, Neumann C, Vowler SL. A longitudinal study on pediatric myringoplasty. Otol Neurotol. 2007 Apr;28(3):353-5. doi: 10.1097/mao.0b013e318030d384, PMID 17414041.
Mangia LR, Amadeu NT, Da Silva Oliveira M, Patzer LS, Somensi ES, Hamerschmidt R. Success rates and predictors of outcomes of type I tympanoplasty performed by residents in a teaching tertiary hospital. J Otol. 2023 Oct;18(4):214-9. doi: 10.1016/j.joto.2023.09.003, PMID 37877068, PMCID PMC10593571.