
Int J Curr Pharm Res, Vol 17, Issue 5, 118-123Original Article
COMPARISON OF CEMENT AUGMENTATION VS NON-AUGMENTED FRACTURE FIXATION OF INTERTROCHANTERIC FEMUR FRACTURE IN ELDERLY PATIENTS
AMANDEEP SINGH BAKSHI, JASPREET SINGH, ABHISHEK, MUKUL SHARMA, MUDIT KUMAR SHARMA, DAVINDER SINGH, HARJAP SINGH, HARRY MEHTA*
Department of Orthopaedics, GMC Patiala, Punjab, India
*Corresponding author: Vankeepuram Vishnu Kalyani; *Email: hk02266@gmail.com
Received: 11 Jun 2025, Revised and Accepted: 01 Aug 2025
ABSTRACT
Objective: To compare the effectiveness of cement-augmented versus non-augmented fixation methods for treating intertrochanteric femur fractures.
Methods: This prospective study was done in a tertiary care hospital of North India on patients presenting with intertrochanteric fractures. After enrolment, the patients using the stringent selection criteria they underwent fracture reduction with and without cement augmentation. Functional assessment utilising the Harris Hip Score (HHS), Quality of life assessment and associated complications were evaluated. Follow-up was done at 6 w, 3 mo, 6 mo and until radiographic union was achieved.
Results: The mean duration of operation was significantly longer in Group I (59.68 min) compared to Group II (49.72 min; p<0.0001). Functional outcomes, assessed using HHS and Barthel index, showed non-significant differences between groups. However, intra-group analyses indicated significant improvements over time. Radiologically, Group II had a significantly greater mean sliding distance of the screw/blade (14.12 mm vs. 12.14 mm; p<0.00001) and higher mean varus deviation (7.16° vs. 3.15°; p<0.0001). Complications were minimal and similar in both groups, with no systemic or thromboembolic complications reported.
Conclusion: The study found significant differences in operative time between the two groups, but functional outcomes were comparable at all follow-up intervals. Radiological analyses revealed significant differences in screw/blade sliding and varus deviation, indicating that cement augmentation may affect biomechanical stability.
Keywords: Intertrochanteric fractures, Cement augmentation, Harris hip score, Barthel index, Sliding
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i5.7070 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Intertrochanteric fracture is a subset of extra-capsular fractures of the proximal femur. It occurs in anatomical region between greater and lesser trochanters [1, 2]. These injuries are predominantly found among older adults, particularly those with osteoporosis, where low-energy mechanisms such as ground-level falls are the primary instigators. In contrast, younger individuals typically sustain these fractures due to high-energy traumas, highlighting the disparate mechanisms underlying their occurrence in different populations. Epidemiologically, studies have documented femaletomale ratio which ranges from 2:1 to 8:1, with affected patients generally older than those presenting with femoral neck fractures, thus underscoring the demographic significance of intertrochanteric falls [3, 4].
The clinical classification of intertrochanteric fractures into stable and unstable categories plays crucial role in both management strategy and prognosis. Stable fractures maintain the integrity of the posteromedial cortex, offering sufficient resistance to compressive forces post-reduction. Conversely, unstable fractures may involve complications such as comminution of the posteromedial cortex, fractures of lesser trochanter, subtrochanteric extensions, or reverse obliquity patterns, which necessitate more complex treatment approaches [5, 6].
Management of intertrochanteric femur fractures is generally stratified into nonoperative treatment and surgical intervention. Although non-operative management is infrequently indicated, it may be suitable for patients who are not able to walk or those at heightened risk of perioperative mortality. However, the associated outcomes tend to be poor, with increased complications such as pneumonia, urinary tract infections, pressure ulcers, and deep vein thrombosis [7, 8]. Surgical management, classified as urgent rather than emergent, allows for optimisation of co morbidities, ultimately reducing morbidity and mortality rates [9].
The predominant surgical techniques include the use of sliding hip screws and intramedullary hip screws, with choice of implant significantly influenced by the fracture pattern and stability [10]. Intramedullary nailing has emerged as a preferred method for more unstable configurations and is favoured for its minimally invasive approach, which potentially reduces intraoperative blood loss. Nevertheless, concerns regarding implant failure, particularly in osteoporotic populations, necessitate the exploration of innovative augmentation techniques [11, 12]. Cement augmentation, utilising materials such as Polymethyl Methacrylate or calcium phosphate, has demonstrated promise in enhancing the mechanical stability of fixation devices, thus improving clinical outcomes [13, 14].
This study compares outcomes of cement-augmented versus non-augmented fixation techniques for intertrochanteric femur fractures in elderly patients. Through this comprehensive analysis, we seek to shed light on the complexities of managing intertrochanteric fractures and their implications for patient care and public health.
MATERIALS AND METHODS
This study is designed as a prospective study conducted in a tertiary care hospital of North India. The trial focuses on patients presenting with unstable intertrochanteric fractures and compares the efficacy of fracture reduction with and without cement augmentation.
Study setting
The study enrolled patients from the emergency and outpatient departments of Orthopaedics between June 2023 and May 2024. The sample size comprised all patients who met predefined selection criteria, and their participation was sanctioned by Institutional Ethics Committee. Written informed consent was taken from all participants.
Inclusion Criteria includes patient’s age ≥65 y and history of low-energy trauma.
Exclusion Criteria includes Age<65 y, History of dementia, Patients with neuromuscular or musculoskeletal deficiencies limiting the ability to perform objective functional tests, Recent history of substance abuse, Active malignancy and concurrent fractures or surgical procedures that could influence postoperative outcomes.
Preoperative assessment
A comprehensive preoperative evaluation was conducted for all enrolled patients, including detailed history taking to ascertain the mechanism of injury and previous medical history, Comprehensive physical and systemic examinations, Clinical assessment specific to the fracture, Radiographic evaluation (X-rays) to confirm fracture site and classification, Necessary routine laboratory investigations (blood and urine tests) for anaesthetic clearance and assessment of the general health of the patient, Computed tomography (CT) scans were conducted as warranted by clinical presentation. All findings were systematically recorded in a designated pro forma.
Randomisation and group allocation
Eligible patients were randomised into two groups of twenty-five each using a computer-generated sequence. Group I underwent fracture reduction with cement augmentation, while Group II received fracture reduction without cement augmentation. All surgical procedures were conducted under spinal anesthesia.
Surgical procedure
Following selection, patients were transported to operating room, where either epidural, spinal, or general anesthesia was administered. Upon successful induction of anesthesia, patients were positioned supine on an orthopaedic fracture table, with uninjured leg secured to a leg holder. Unlike positioning required for using DHS, it was essential to adduct ipsilateral hip to facilitate nail entry; this was achieved by tilting torso 10 to 15 degrees toward the contralateral side.
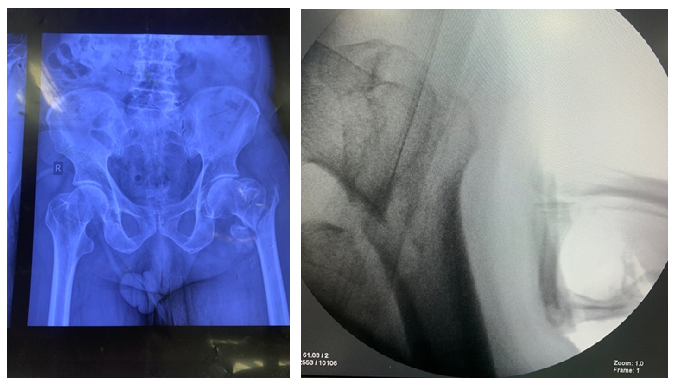
Fig. 1: Left IT femur #
Initially, closed reduction was attempted using internal rotation and longitudinal traction. In cases where closed reduction was not feasible, a mini-open approach was employed. This involved making a small longitudinal incision approximately 5 cm proximal to greater trochanter. Gluteal fascia was incised, and gluteus medius was split longitudinally to access tip of trochanter. The correct entry point for nail was determined using fluoroscopy, and a guide wire was advanced from trochanter to medulla (fig. 2).
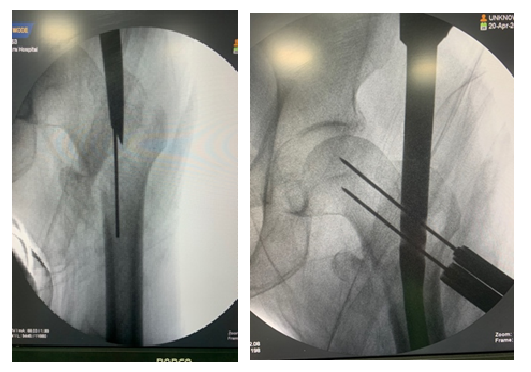
Fig. 2: Entry site
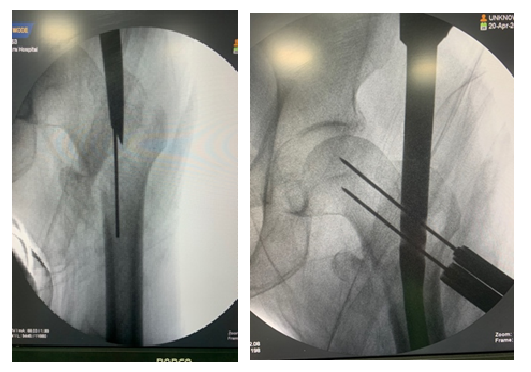
Fig. 3: Lag screw guide wire placed close to calcar
Subsequently, a cannulated drill was used to establish an entry point for nail. After drilling the proximal femur, a nail sized at 130° and 240 mm was inserted. Under fluoroscopic guidance, lag screw guides were positioned as near to the calcar as possible on the anteroposterior radiograph and centrally on lateral radiographs (fig. 3).
Once the appropriate location was identified, measurements were recorded. A novel cement inserter device was developed based on diameter of PFNA instrumentation (fig. 4)

Fig. 4: Cement inserter device

Fig. 5: Bone cement
After obtaining necessary measurements, poly methyl methacrylate (PMMA) (fig. 5) bone cement was prepared, and using newly designed device, the cement was inserted (in doughy state) into the femoral head through predrilled screw site under fluoroscopic supervision (fig. 6).
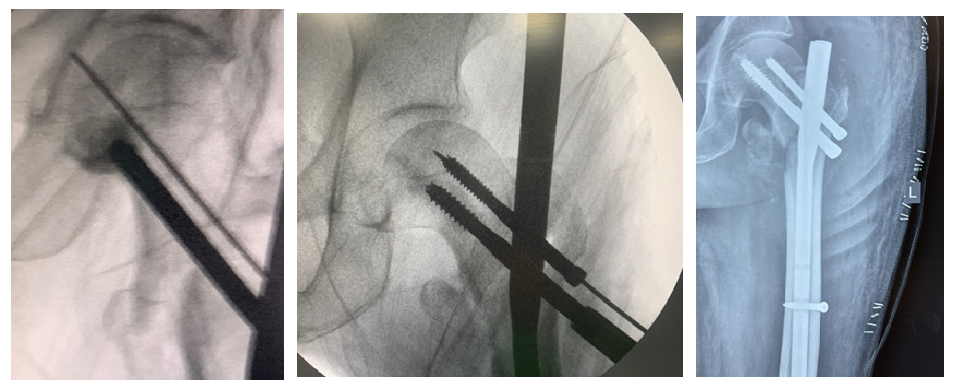
Fig. 6: Cement inserted
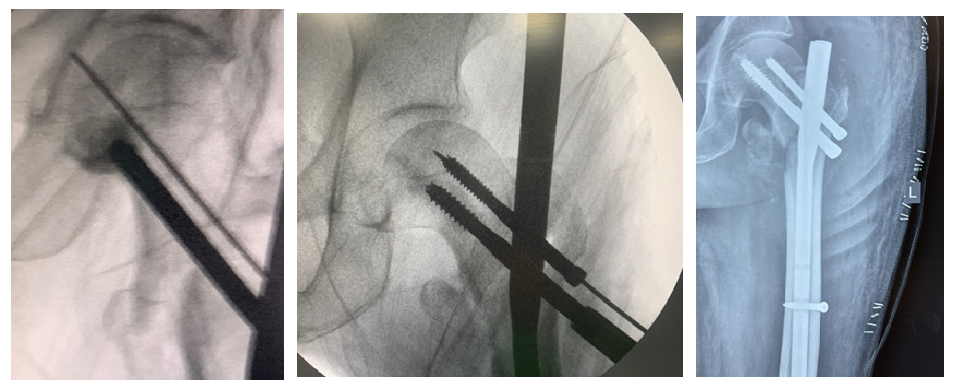
Fig. 7: Screw inserted
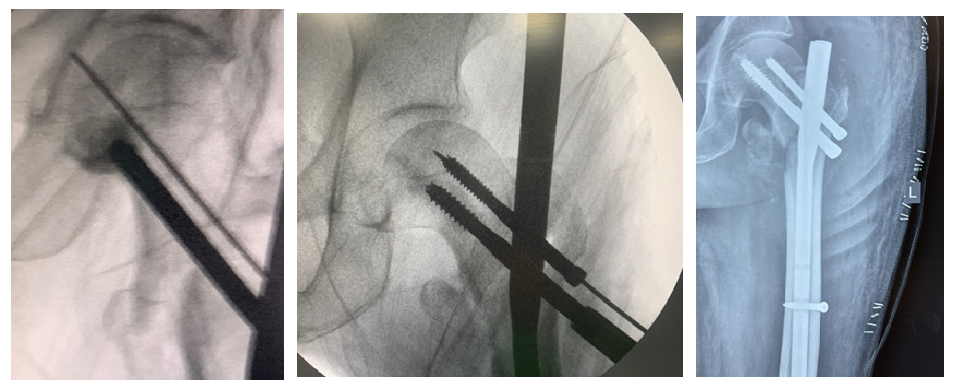
Fig. 8: Post op x-rays
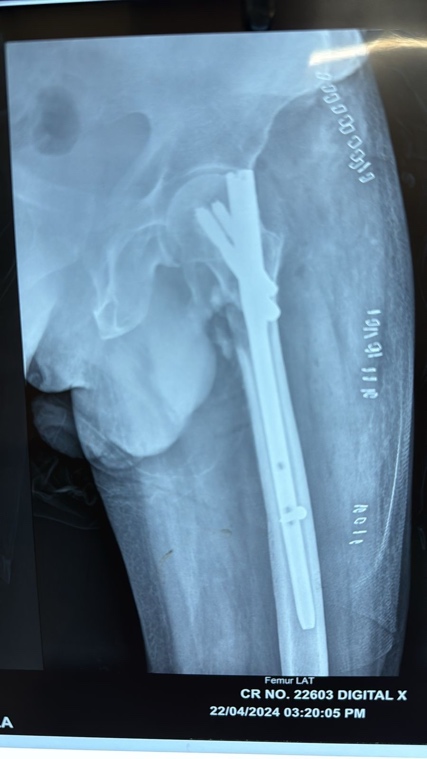
Fig. 9: Post op X-rays

Fig. 10: Post op X-rays (2nd)
Upon completion of cement insertion, the appropriately sized screw was inserted without any time delay following insertion of cement, followed by derotation screw (fig. 6,7). In none of the case we notices loss of reduction and fixation during whole of the process. The nail was statically locked distally with one screw. Postoperative management included standard prophylaxis for deep vein thrombosis, and patients were mobilised with weight-bearing as tolerated and no cement related complications were noted.
Follow-Up and outcome measures
Patients were scheduled for follow-up assessments at 6 w, 3 mo, 6 mo, and until radiographic union was achieved. During these follow-ups, evaluations focused on: Healing of the postoperative incision and any adverse symptoms, Radiographic assessment (X-rays) to evaluate bone healing, specifically at the 3-month mark.
Outcome measures
Primary Outcome Measures include Functional assessment utilising HHS, Quality of life assessment, Rate of complications categorised into implant-related, systemic, and thromboembolic complications.
Secondary Outcome Measures include Re-interventions required at the fracture site during the follow-up period, Radiological outcomes, specifically measuring screw/blade migration in millimetres (mm) on AP X-rays and varus angulation in degrees as observed in the same radiographs.
Statistical analysis plan
The collected data were compiled and analysed using the Statistical Program for Social Sciences (SPSS) software version 20.0 (Chicago, Illinois, USA). Statistical analyses were conducted on an intention-to-treat basis.
RESULTS
Demographic and clinical characteristics
The study evaluated a total of fifty patients diagnosed with unstable intertrochanteric fractures, distributed into two groups: Group I (n=25) received fracture reduction with cement augmentation, while Group II (n=25) underwent standard fracture reduction without cement augmentation.
The mean age of participants in Group I was 71.80±6.88 y (range, 65-89 y), compared to 71.36±7.39 y (range, 65-89 y) in Group II. Statistical analysis revealed no significant difference in age between the two groups (p = 0.8284). Gender distribution showed that Group I consisted of 14 females (56%) and 11 males (44%), whereas Group II included 7 females (28%) and 18 males (72%). The difference in gender distribution was statistically significant (p = 0.0448).
Co morbidities were present in 23 patients (92%) in Group I and 22 patients (88%) in Group II, with no statistically significant difference observed (p = 0.6373).
Operative time
The mean operative time was significantly longer in Group I at 59.68±7.25 min (range, 42-78 min) compared to 49.72±6.15 min (range, 40-62 min) in Group II. This difference was statistically significant (p<0.0001).
Functional outcomes
At 6 w postoperatively, the mean Harris Hip Score (HHS) for Group I was 50.80±20.38 (range, 18-88) and for Group II was 50.68±19.95 (range, 18-84), indicating no significant difference between the two groups (p = 0.9833). At the 3-month follow-up, the mean HHS in Group I was 56.72±18.87 (range, 25-85) and in Group II was 53.24±19.37 (range, 24-87), again showing no significant difference (p = 0.5230). At 6 mo, patients in Group I had a mean HHS of 57.24±18.21 (range, 27-87), while Group II had a mean HHS of 55.12±16.90 (range, 30-84) (p = 0.6716). Upon complete union, the mean HHS was 60.48±17.26 (range, 31-88) for Group I and 56.00±17.51 (range, 32-85) for Group II; the difference remained statistically non-significant (p = 0.3669).
Intra-group comparisons of the HHS indicated that the differences were statistically nonsignificant in both groups (p>0.05).
Quality of life assessment
The Barthel index scores at 6 w postoperatively revealed a mean of 62.68±9.72 (range, 26-75) for Group I and 61.08±9.45 (range, 30-73) for Group II (p = 0.5579; non-significant). At 3 mo, the scores were 75.64±11.03 (range, 33-87) for Group I and 72.92±10.88 (range, 36-82) for Group II (p = 0.3843). At the 6-month mark, patients in Group I exhibited a mean Barthel index of 81.12±9.89 (range, 39-89) compared to 81.68±11.61 (range, 39-90) for Group II (p = 0.8551). Upon complete union, the mean Barthel index scores were 81.56±8.61 (range, 43-89) in Group I and 83.76±11.29 (range, 42-91) in Group II (p = 0.4424), indicating no significant difference.
However, intra-group analyses of the Barthel index indicated highly significant differences over time for both groups (p<0.00001).
Complications
Complications related to fractures or implants were noted in one patient (4%) in each group. Importantly, there were no reported cases of systemic or thromboembolic complications in either group throughout the study period.
Table 1: Baseline characteristics of patients
| Patients | Group I | Group II | Significance level |
| Age | 71.80±6.88 y | 71.36±7.39 y | 0.8284 (NS) |
| Gender | Male (44%) Female (56%) | Male (72%) Female (28%) | 0.0448 (NS) |
| Operative time (Minutes) | 59.68±7.25 | 49.72±6.15 | <0.0001 (HS) |
| Co morbidities | 92% | 88% | 0.6373 (NS) |
Table 2: Comparison of outcomes
| Timelines | Group I | Group II | Significance level (Inter-group) | |
| Harris Hip score | 6 w | 50.80±20.38 | 50.68±19.95 | 0.9833 (NS) |
| 3 mo | 56.72±18.87 | 53.24±19.37 | 0.5230 (NS) | |
| 6 mo | 57.24±18.21 | 55.12±16.90 | 0.6716 (NS) | |
| At complete union | 60.48±17.26 | 56.0±17.51 | 0.3669 (NS) | |
| p-Value (Intra-group) | 0.3290 (NS) | 0.7492 (NS) | ||
| 6 w | 62.68±9.72 | 61.08±9.45 | 0.5579 (NS) | |
| Barthel index | 3 mo | 75.64±11.03 | 72.92±10.88 | 0.3843 (NS) |
| 6 mo | 81.12±9.89 | 81.68±11.61 | 0.8551 (NS) | |
| At complete union | 81.56±8.61 | 83.76±11.29 | 0.4424 (NS) | |
| p-Value (Intra-group) | <0.00001 (HS) | <0.00001 (HS) | ||
| Sliding distance (mm) | 12.14±1.27 | 14.12±1.28 | <0.0001 (HS) | |
| Varus deviation | 4.46°±1.21 | 7.16°±1.44° | <0.0001 (HS) |
*ANOVA test applied
Radiological outcomes
The mean sliding distance of the screw/blade was significantly greater in Group II at 14.12±1.28 mm (range, 12.22-16.78 mm) compared to 12.14±1.27 mm (range, 10.32-14.54 mm) in Group I, yielding a highly significant difference (p<0.00001).
Moreover, the mean varus deviation was significantly higher in Group II at 8.03°±0.60° (range, 7.02-9.34°) compared to 4.10°±0.59° (range, 3.80-5.20°) in Group I, with this difference also being statistically highly significant (p<0.0001).
DISCUSSION
In our study, the outcomes of cement augmentation versus non-augmentation in unstable intertrochanteric fractures in elderly patients was evaluated. The demographic profile of the participants revealed a similar age distribution between the two groups(p = 0.8284; non-significant). However, the gender distribution indicated a notable preponderance of males in Group II and a predominance of females in Group I (p = 0.0448; significant). This finding mirrors reports from Ahmed RM (2024) [15] and Fidan F et al. (2022) [16], which highlight the typical demographic characteristics (The age ranged from 44 to 90 y, with a mean age of 73) associated with hip fracture cases.
Co-morbidities were prevalent in both groups, affecting 92% of patients in Group I and 88% in Group II (p = 0.6373; non-significant). These rates are in line with findings from Kulachote N et al. (2020) [17], suggesting that patients with complex medical histories are frequently encountered in this demographic.
Our study found a significant difference in operative time, with Group I demonstrating a longer mean duration (59.68±7.25 min) compared to Group II (49.72±6.15 min), indicating a considerable impact of cement augmentation on surgical time (p<0.0001). These findings contrast with previous studies, such as those by Mochizuki Y et al. (2022) [18], which also noted no significant difference in operative times between augmented and non-augmented groups.
Functional assessments, including HHS and Barthel Index, revealed no significant differences at different follow-ups postoperatively, despite both groups showing improvement over time. The intra-group comparisons for both HHS and Barthel Index demonstrated statistically significant improvements (p<0.00001), supporting the efficacy of surgical intervention for enhancing mobility and independence, regardless of the augmentation approach. These results are similar to findings from Keppler AM et al. (2021) [19] and Kammerlander C et al. (2018) [20], who also documented comparable outcomes between surgical techniques.
Radiological outcomes further emphasised the advantages of cement augmentation. The significant differences in mean sliding distance of the screw/blade (12.14 mm in Group I vs. 14.12 mm in Group II; p<0.00001) and varus deviation (4.46° in Group I vs. 7.16° in Group II; p<0.0001) underscore the enhanced stability afforded by augmentation. These findings are consistent with reports of reduced sliding distances and varus collapsein augmented groups, such as those documented by Kim SJ et al. (2018) [21] and Mattsson P et al. (2004) [22], indicating potential implications for improved structural integrity and reduced risk for re-fracture or complications.
Regarding postoperative complications, the incidence of fracture or implant-related complications was low and equivalent between the two groups (4% each). This compares favourably with the higher complication rates reported by Ahmed RM (2024) [15] and Kim SJ et al. (2018) [21], suggesting that cement augmentation may lead to fewer complications in certain contexts when compared to other studies. Aligning with this study, Stramazzo l et al. (2021) observed no significant complications [13].
This study's limitations include its relatively short follow-up duration, small sample size, and the region-specific nature of data collected, which may limit generalisability. Additionally, selection bias was a concern, as only mobilised patients prior to fracture were included, potentially excluding those with higher degrees of osteoporosis who might benefit from PFNA augmentation.
CONCLUSION
The findings from this study demonstrate that while operative time differed significantly between the two groups, functional outcomes as measured by HHS and Barthel index scores were statistically comparable at all follow-up intervals. Radiological analyses indicated significant differences in screw/blade sliding and varus deviation, suggesting a potential impact of cement augmentation on biomechanical stability. Future multi-centric studies with larger sample sizes will enhance the robustness of the findings and allow for broader application of the results to diverse patient populations.
ACKNOWLEDGEMENT
None
PATIENT CONSENT
Written informed consent has been obtained from the patient or guardian for participation and publication.
ETHICAL APPROVAL AND CONSENT
Approval was taken from the relevant ethics committee and written informed consent was taken from each patient to publish his details while maintaining confidentiality.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICTS OF INTERESTS
Declared none
REFERENCES
Karakus O, Ozdemir G, Karaca S, Cetin M, Saygi B. The relationship between the type of unstable intertrochanteric femur fracture and mobility in the elderly. J Orthop Surg Res. 2018 Aug 22;13(1):207. doi: 10.1186/s13018-018-0911-1.
Sharma A, Sethi A, Sharma S. Tratamento de fraturas intertrocantericas estaveis do femur com haste femoral proximal versus parafuso dinamico de quadril: um estudo comparativo. Rev Bras Ortop. 2018 Jul-Aug;53(4):477-81. doi: 10.1016/j.rbo.2017.07.002.
Kani KK, Porrino JA, Mulcahy H, Chew FS. Fragility fractures of the proximal femur: review and update for radiologists. Skelet Radiol. 2019 Jan;48(1):29-45. doi: 10.1007/s00256-018-3008-3.
Amini MH, Feldman JJ, Weinlein IV JC. High complication rate in young patients with high-energy intertrochanteric femoral fractures. Orthopedics. 2017 Mar 1;40(2):e2939. doi: 10.3928/01477447-20161128-04.
Zamboni DR. Intertrochanteric fractures. In: Slullitel P, Rossi L, Camino Willhuber G, editors. Orthopaedics and trauma: current concepts and best practices. Berlin: Springer International Publishing; 2024. p. 467-75. doi: 10.1007/978-3-031-30518-4_37.
Attum B, Pilson H. Intertrochanteric femur fracture. In: Treasure Island, FL: StatPearls Publishing; 2023 Aug 8. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493161/.
Tronzo RG. Special considerations in management. Orthop Clin North Am. 1974;5(3):571-83. doi: 10.1016/S0030-5898(20)31057-9.
Wang F, Meng C, Cao XB, Chen Q, Xu XF, Chen Q. Hemiarthroplasty for the treatment of complicated femoral intertrochanteric fracture in elderly patients. Zhongguo Gu Shang. 2018 Sep 25;31(9):818-23. doi: 10.3969/j.issn.1003-0034.2018.09.008, PMID 30332874.
Carpintero P. Complications of hip fractures: a review. World J Orthop. 2014 Sep 9;5(4):402. doi: 10.5312/wjo.v5.i4.402.
Bartonicek J. Trochanteric fractures: sliding hip screw. Fractures of the proximal femur: improving outcomes: expert consult; 2010 Sep 24. p. 113.
Sivananthan S, Goodman SB, Burke M. Failure mechanisms in joint replacement. In: Joint replacement technology. Elsevier; 2021. p. 373-402. doi: 10.1016/B978-0-12-821082-6.00017-0.
Gunaki RB, Deokar NP, Sudaryanto A. Shraddha Naik Bahulekar. Adv Clin Med; 2024 May 1. p. 228.
Stramazzo L, Ratano S, Monachino F, Pavan D, Rovere G, Camarda L. Cement augmentation for trochanteric fracture in elderly: a systematic review. J Clin Orthop Trauma. 2021;15:65-70. doi: 10.1016/j.jcot.2020.10.034, PMID 33717919.
Von Der Linden P, Gisep A, Boner V, Windolf M, Appelt A, Suhm N. Biomechanical evaluation of a new augmentation method for enhanced screw fixation in osteoporotic proximal femoral fractures. J Orthop Res. 2006;24(12):2230-7. doi: 10.1002/jor.20299, PMID 17001708.
Ahmed RM. Evaluating the impacts of proximal femoral nail anti-rotation (PFNA) augmentation in osteoporotic intertrochanteric fractures. Am J Med Sci Innov. 2024 May 15;3(1):96-106. doi: 10.54536/ajmsi.v3i1.2758.
Fidan F, Lapcin O. Outcomes of osteoporotic intertrochanteric fractures treated with cement augmented proximal femoral nail. J Surg Med. 2022;6(10):854-7. doi: 10.28982/josam.7445.
Kulachote N, Sa Ngasoongsong P, Sirisreetreerux N, Chulsomlee K, Thamyongkit S, Wongsak S. Predicting factors for return to prefracture ambulatory level in high surgical risk elderly patients sustained intertrochanteric fracture and treated with proximal femoral nail antirotation (PFNA) with and without cement augmentation. Geriatr Orthop Surg Rehabil. 2020 Mar 12;11. doi: 10.1177/2151459320912121.
Mochizuki Y, Yamamoto N, Fujii T, Tomita Y. Effectiveness of cement augmentation on early postoperative mobility in patients treated for trochanteric fractures with cephalomedullary nailing: a prospective cohort study. J Pers Med. 2022 Aug 27;12(9):1392. doi: 10.3390/jpm12091392, PMID 36143177.
Keppler AM, Pfeufer D, Kau F, Linhart C, Zeckey C, Neuerburg C. Cement augmentation of the proximal femur nail antirotation (PFNA) is associated with enhanced weight bearing in older adults. Injury. 2021 Oct 1;52(10):3042-6. doi: 10.1016/j.injury.2021.01.037, PMID 33583593.
Kammerlander C, Hem ES, Klopfer T, Gebhard F, Sermon A, Dietrich M. Cement augmentation of the proximal femoral nail antirotation (PFNA) a multicentre randomized controlled trial. Injury. 2018 Aug 1;49(8):1436-44. doi: 10.1016/j.injury.2018.04.022.
Kim SJ, Park HS, Lee DW, Lee JW. Is calcium phosphate augmentation a viable option for osteoporotic hip fractures? Osteoporos Int. 2018 Sep;29(9):2021-8. doi: 10.1007/s00198-018-4572-z.
Mattsson P, Larsson S. Unstable trochanteric fractures augmented with calcium phosphate cement: a prospective randomized study using radiostereometry to measure fracture stability. Scand J Surg. 2004;93(3):223-8. doi: 10.1177/145749690409300310.