
Int J Curr Pharm Res, Vol 17, Issue 4, 69-73Original Article
COMPARISON OF POSTOPERATIVE ANALGESIC EFFICACY OF ROPIVACAINE WITH DEXAMETHASONE VERSUS ROPIVACAINE WITH DEXMEDETOMIDINE IN TRANSVERSUS ABDOMINIS PLANE BLOCK IN INGUINAL HERNIA REPAIR
KARTHIK KUMAR V.*, PYDIMALLA VENKATA GOWTHAM, KARUNA KUMAR DAS
Department of Anaesthesiology, Assam Medical College and hospital, Dibrugarh, Assam, India
*Corresponding author: Karthik Kumar V.; *Email: karthikvelu1304@gmail.com
Received: 15 Apr 2025, Revised and Accepted: 10 Jun 2025
ABSTRACT
Objective: The aim of this study was to assess the efficacy of addition of dexamethasone or dexmedetomidine to ropivacaine in Transversus Abdominis Plane (TAP) block for post‑operative pain relief in inguinal hernia repair.
Methods: Seventy-two patients (18–45 y) of American Society of Anaesthesiologists (ASA) grade I-II undergoing elective inguinal hernia repair were randomly divided into two groups. After completion of surgery under spinal anaesthesia, patients received ultrasound‑guided (USG) TAP block with 20 ml of 0.25% ropivacaine along with 2 ml of 0.1 mg/kg dexamethasone (Group I) or 2 ml of 1μg/kg dexmedetomidine (Group II) in this study. Visual analogue scale (VAS) for pain, time to initial self‑reporting of post‑operative pain, time to first rescue analgesic demand, haemodynamic parameters and adverse effects if any were notedanda P value<0.05 was considered as statistically significant.
Results: The mean VAS score was comparable between two groups for the first four hours, but it was significantly lower at 6,12and18 h in group II. Duration of analgesia was significantly longer in group II (410.25±18.2vs. 520.52±12.3 min, P<0.001) and total opioid consumption in 24 h (150.43±32.21 vs 98.80±4.2 mg, P<0.001) was significantly lower in group II as compared to group I. Significant fall in HR was observed at 2,4 and 6 h in group II which didn’t require any medical intervention.
Conclusion: Addition of dexmedetomidine to ropivacaine as compared with dexamethasone in USG guided TAP block following inguinal hernia repair prolongs the time to initial post‑operative pain and time to first rescue analgesic consumption with less significant side effects.
Keywords: Ropivacaine, Dexamethasone, Dexmedetomidine, TAP block
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i4.7014 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
One of the most popular surgical procedures-Inguinal hernioplasty is associated with moderate to severe postoperative pain. Acute postoperative pain is harmful because it exacerbates the patient's discomfort and associated with prolonged hospital stay and delayed return to normal daily activities [1]. To manage post-operative pain, various modalities are available which include pharmacological methods, topical analgesics, peripheral nerve blocks with local anaesthetics (LA), epidural analgesia and non-pharmacological approaches [2].
Transversus Abdominis Plane (TAP) block is the regional anaesthetic compartment block effective in abdominal surgeries in which LA are deposited to block thoracolumbar nerves T6 to L1 supplying parietal peritoneum as well as the skin and muscles of anterior abdominal wall by traversing through the plane between layers of transversus abdominis and internal oblique muscles of abdomen (Transversus abdominis plane). It provides adequate postoperative analgesia following various abdominal surgeries [3-5]. As the use of ultrasound in blocks improves the success rate, reduces the volume of LA and prevents injury to adjacent structures, which occurs with blind technique, USG guided TAP block is employed in our study [6].
The duration of the block can be extended if LA can be administered via an infusion catheter, which is associated with its own complications. In order to extend the effects of LA, adjuvant drugs such as dexamethasone, magnesium sulphate, and dexmedetomidine can be used [7].
Ropivacaine, a local anaesthetic agent which has similar efficacy, greater safety and lower toxic profile when compared to bupivacaine. Dexmedetomidine is a selective alpha‑2 (α2) adrenergic receptor agonist which prolongs the effect of the LA when given intrathecally, epidurally and in peripheral nerve blocks [8].
Dexamethasone is a corticosteroid drug which inhibits the potassium channel-mediated discharge of nociceptive C-fibres reducing ectopic neuronal discharge and local vasoconstriction by acting on glucocorticoid receptors that tends to increase the duration of analgesia whenever administered either perineurally or intravenously [9].
Despite an extensive review of the literature, very few resources were found comparing dexamethasone and dexmedetomidine as adjuvants to ropivacaine in TAP blocks for inguinal hernia repair and according to previous studies, there are contradictory results regarding the overall efficacy of these two additives as adjuvants in LA. Therefore, we conducted our study using ropivacaine as a local anaesthetic and dexamethasone or dexmedetomidine as an adjuvant in TAP block.
The aim of this study is to determine the postoperative analgesic efficacy of dexamethasone and dexmedetomidine as an adjuvant to ropivacaine in TAP block in patients undergoing inguinal hernia repair under spinal anaesthesia.
Primary objective
To assess and compare the analgesic efficacy of dexamethasone and dexmedetomidine when used as an adjuvant to ropivacaine in TAP block using VAS score.
Secondary objectives
To assess and compare the post-operative duration of analgesia, post-operative opioid requirements, hemodynamic profile and associated side effects with these two adjuvants in TAP block.
MATERIALS AND METHODS
After taking Institutional Ethical Committee (H), AMCH, Dibrugarh approval, this study was conducted in ASA Grade I-II patients of age 18-35 y posted for elective inguinal hernia repair surgeries under subarachnoid block during the period from January 2025 to march 2025.
Inclusion criteria
Male Patients aged between 18 – 35 y with weight of 60 to 75 kg and height 160 cm to 175 cm
Exclusion criteria
Patient refusal, ASA grade III and IV, infection at the site of injection, Coagulopathy or anticoagulant drugs, obstructed and strangulated hernia, Intraoperative requirement of additional analgesia or GA, Patients on chronic analgesics and history of allergy to study drugs.
After a detailed pre-anaesthetic check-up including routine investigations, patients who fulfilled the inclusion criteria were included in the study and written informed consent was obtained from all those patients. All the patients were randomly allocated using computer-generated random numbers contained in sequentially sealed envelopes into two groups of thirty-six each. The study medication was concealed from the observer anaesthesiologist who gathered the postoperative data. A nonparticipant staff member prepared and delivered the study medication solution to the investigator.
The group I received 20 ml of 0.25% ropivacaine and 2 ml of 0.1 mg/kg dexamethasone and group II received 20 ml of 0.25%ropivacaine and 2 ml of 1 μg/kg dexmedetomidine.
A standardized anaesthesia protocol was followed for all patients. Under aseptic precautions, spinal anaesthesia was administered using 3.2 ml of 0.75%ropivacaine (hyperbaric) at L3–4 interspace with 25-gauge Quincke tip Spinal needle. Electrocardiogram, oxygen saturation with pulse oximeter (SpO2) and non‑invasive blood pressure were monitored continuously and were recorded every 5 min during the intraoperative period. Surgery started after confirming adequate level of Anaesthesia (T6).
Following surgery and block regression to the T10 dermatomal level, both the groups received USG-guided Transversus Abdominis Plane block utilizing a linear probe (6–13 MHz) and the appropriate drug solutions. Under aseptic precautions, 23 G spinal needle was advanced using an ultrasound-guided in-plane technique at the anterior axillary line between the 12th rib and iliac crest, with the umbilicus at the centre. The precise location of the needle tip in a plane between the internal oblique muscle and the transverse abdominis muscle was determined using 1 ml of normal saline. After confirmation of hypoechoic area on USG imaging, the injection of 22 ml of drug solution was given. Postoperatively, the patients were evaluated in post-anaesthesia care unit at 0, 2, 4, 6, 12, 18 and 24 h by an investigator blinded to group assignment. Pain level (somatic and visceral) at rest and on movement (knee flexion) was quantified with VAS pain scale (0 = no pain and 10 = worst pain) postoperatively for 24h at mentioned time intervals.
Time to demand of first supplementary analgesic request was considered as duration of analgesia of TAP block and further rescue analgesia was administered to patients if VAS score>4. Inj. Tramadol 1 mg/kg was administered as rescue analgesia and the total opioid (rescue analgesia) consumption in mg given also noted.
Any side effects like Nausea, vomiting and sedation were assessed for the first 24 h. Level of sedation was assessed using Ramsay sedation score and patients were considered sedated if score>4.
Outcome
Primary outcome measures
To assess the severity of post-operative pain between both the groups at various intervals using VAS score.
Secondary outcome measures
1. To measure the duration of analgesia and post-operative opioid requirements between both the groups
2. To assess and compare the hemodynamic profile and the incidence of side effects between both the groups.
Statistical analysis
Considering the VAS score at 6, 9 and 12 h which were significant of levobupivacaine with dexamethasone are3.06±1.96, 2.39± 1.93 and 1.67±1.59 and levobupivacaine with dexmedetomidine are 1.72± 1.61, 0.92±1.52 and 0.69± 1.24 respectively [10], after adding a non-response rate of 10%, sample size for present study is calculated and rounded off to be 36 (highest value among the three sample size) in each group with 95%confidence and 90% power.
The statistical analysis of data was performed using the computer program, Statistical Package for Social Sciences (SPSS for Windows, version 20.0. Chicago, SPSS Inc.) and Microsoft Excel 2010. Results on continuous measurements were presented as mean±standard deviation are compared using student t test. Discrete data were expressed as number (%) and were analysed using Chi square test and Fischer’s exact test (where the cell counts were<5 or 0). For all analyses, the statistical significance was fixed at 5% level (p value<0.05).
RESULTS
Demographic variables such as age, weight, height, ASA status and the duration of the surgery between two groups were comparable and no statistically significant differences were found (table 1)
Table 1: Demographic data’s
| Parameters | Group I | Group II | P value |
| Age (years) | 27.04±3.40 | 28.50±7.75 | 0.306 |
| Weight (kg) | 67.30±9.73 | 68.23±5.20 | 0.615 |
| Height (cm) | 168.50±4.50 | 170.45±6.30 | 0.136 |
ASA status Grade-I Grade-II |
15 (41.67%) 21(58.33%) |
17(47.22%) 19 (52.78%) |
0.64 |
| Duration of surgery (mins) | 90.12±2.66 | 91.35±4.20 | 0.143 |
The mean VAS score for pain was zero in both the groups at 0 and 2 h and there was comparable mean VAS score at 4 hin group I(1.2±4.22) in comparison to group II (0.6±1.85)– P value of 0.44. The mean VAS score was statistically significant at 6 h between group I and II (2.95±1.68, vs 1.90±1.47, p value 0.006**) and at 12 h (3.68±2.0 vs 2.52±1.38, p value 0.005**). At 18 h, the mean VAS score was 3.12±1.28 in group I and 2.03±1.72 in group II, which was statistically significant with p value of 0.003** and at 24 h, the mean VAS score was comparable between both the groups (fig. 1).
Table 2: Comparison of duration of analgesia and total opioid consumption between two groups
| Duration | Group I | Group II | P value |
| Duration of Analgesia (min) | 410.25±18.2 | 520.52±12.3 | <0.001** |
| Total opioid consumption (mg) in 24 h | 150.43±32.2 | 98.80±4.2 | <0.001** |
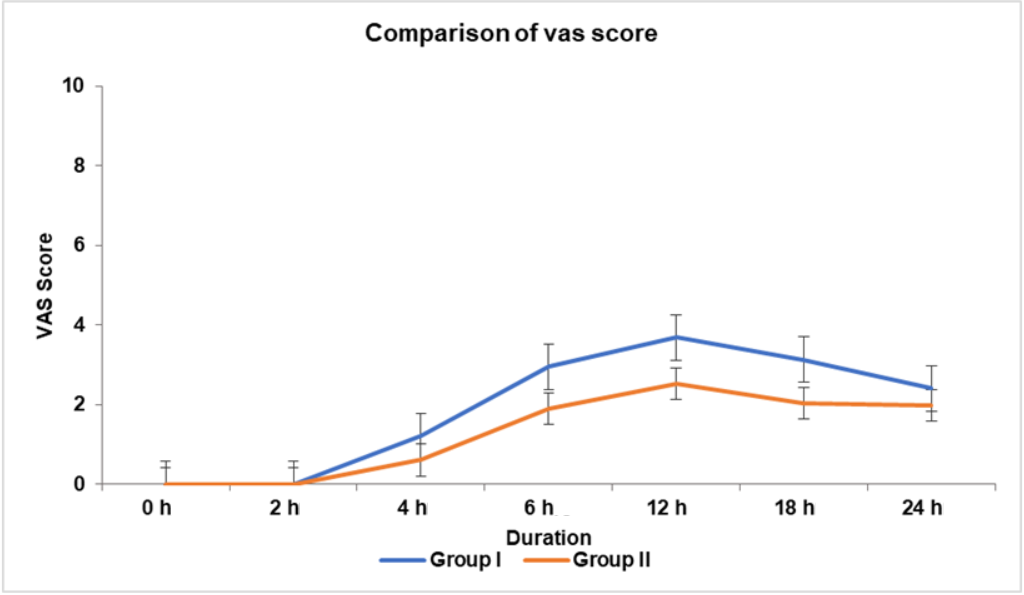
Fig. 1: Comparison of vas score between two groups
The time for first rescue analgesia is considered as the duration of analgesia, which was 410.25±18.2 min in Group I and 410.25±18.2 min in group II and these differences between two groups were statistically very significant (P value<0.001). The total opioid consumption (mg) in 24 h is 200.43±32.2 mg in group I and 98.80±4.2 mg in group II and these differences between two groups were statistically very significant (P value<0.001).
Hemodynamic parameters
Heart rate (HR) and mean arterial pressure (MAP) were recorded at 0,2,4,6,12,18,24 h. Statistically significant decrease in HR was found in group II at 2,4 and 6 h compared to group I (p value<0.05) as shown in table 3. The differences in MAP between two groups were statistically insignificant except at 4 h where the p-value was 0.037 (table 4).
Table 3: Comparison of mean heart rate between two groups
| Duration | Group I | Group II | P value |
| 0 h | 78.52±13.6 | 75.53±8.7 | 0.23 |
| 2 h | 77.35±15.9 | 70.27±3.2 | 0.011* |
| 4 h | 75.16±9.8 | 68.32±11.2 | 0.007** |
| 6 h | 73.25±4.5 | 68.02±4.56 | <0.001** |
| 12 h | 73.02±6.30 | 71.53±3.52 | 0.22 |
| 18 h | 75.48±12.3 | 74.30±8.62 | 0.64 |
| 24 h | 78.09±7.35 | 76.43±5.62 | 0.288 |
Table 4: Comparison of mean arterial pressure between two groups
| Duration | Group I | Group II | P value |
| 0 h | 85.42±9.08 | 84.30±9.03 | 0.60 |
| 2 h | 84.55±9.96 | 81.02±8.64 | 0.11 |
| 4 h | 84.02±8.72 | 79.94±7.52 | 0.037* |
| 6 h | 85.25±12.14 | 81.23±6.78 | 0.087 |
| 12 h | 85.57±10.12 | 82.54±11.32 | 0.234 |
| 18 h | 86.02±8.82 | 83.94±9.54 | 0.340 |
| 24 h | 85.63±6.34 | 84.28±8.22 | 0.438 |
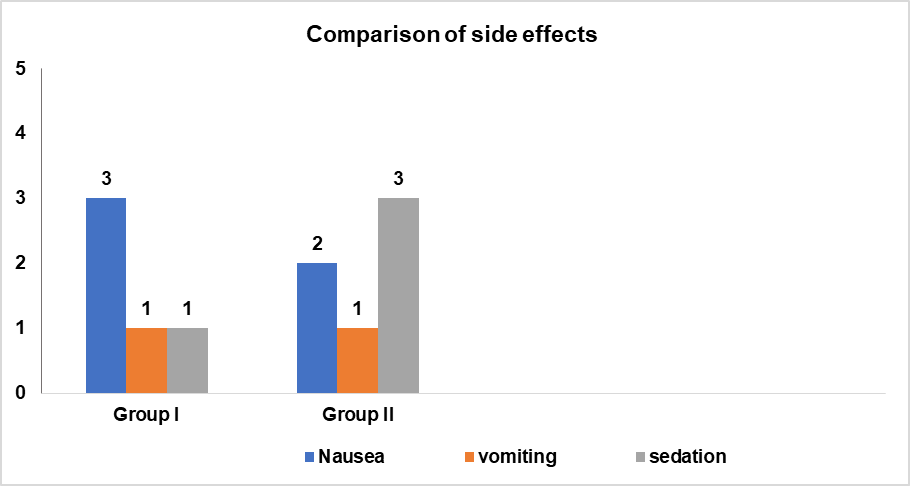
Fig. 2: Comparison of side effects between two groups
The side effects like Nausea was observed in3 patients (8.3%) in group I and 2 patients (5.5%)in group II and incidence of vomiting was similar in both groups (only 1 patient (2.7%)). 1 patient (2.7%) in group I and 3 patient (8.3%) in group II were found to be sedated. No significant differences in side effects were found between two groups (p value>0.05).
DISCUSSION
The TAP block provides effective postoperative analgesia, which is affordable, requires less skill and lowers opioid use in the post-operative phase. A randomised control trial performed by Aguirre-Ospina OD et al. [11] demonstrated the effectiveness of TAP block in providing postoperative analgesia in inguinal hernia repair.
Given that IV doses of less than 0.1 mg/kg did not result in any opioid-sparing effect and that Desmet et al. study [12] found that IV and perineural dexamethasone are equally effective at extending the analgesic duration of regional anaesthesia, Dexamethasone is used in dose 0.1 mg/kg as an additive to ropivacaine in this study to prolong the duration of analgesia.
As per a study conducted by Madangopal, et al. [13], which compared two different doses of dexmedetomidine as an adjuvant to bupivacaine in TAP block, 0.5 µg/kg dexmedetomidine was used as an additive to ropivacaine in our study, which prolonged analgesic effect.
In our study, we found no significant difference in age, weight, height, ASA status, duration of surgery between two groups.
Vas score
The mean VAS score until initial four hours were comparable between both groups, which could be due to residual effects of subarachnoid block. But VAS score was significantly lower in patients who received dexmedetomidine (group-II) compared to patients who received dexamethasone (group I) at 6, 12 and 18 h. This can be explained with the fact that dexmedetomidine with ropivacaine prolongs the duration of TAP block by inhibition of hyperpolarization-activated cationic current and via vasoconstriction [14].
Jyoti Sinha et al. [10] conducted a study in which levobupivacaine with adjuvants dexamethasone and dexmedetomidine used for TAP block for total abdominal hysterectomies also showed decreased VAS score in patients received dexmedetomidine as an adjuvant.
Rescue analgesia
The time to first recue analgesia is prolonged with dexmedetomidine group (group II) and earlier in dexamethasone group (group I) in our study.
In a different trial conducted by Nitika Singla et al. [15], ropivacaine was used in conjunction with either dexmedetomidine or dexamethasone as two distinct adjuvants in TAP block for postoperative analgesia following caesarean delivery. They found that the group receiving ropivacaine with dexmedetomidine had a longer latency to initial rescue analgesia.
In our study, the total opioid consumption was also found to be comparatively more in group I than group II. Similar results with decreased rescue analgesia consumption among patients who received dexmedetomidine as adjuvant in TAP block was also found in study conducted by Thakur J et al. [16], Elhamamy N et al. [17].
Hemodynamic parameters
Significant fall in mean HR from baseline was found at 2,4 and 6 h in patients of group II and significant fall in MAP was observed at 4 h in group II, which can be explained with central alpha-2 agonistic action of dexmedetomidine. No such fall in heart rate and MAP was observed in group I (dexamethasone group).
Similar hemodynamic profile was observed in a trial conducted by Madangopal et al. [12] with two different doses of dexmedetomidine as adjuvant to bupivacaine in TAP block.
Side effects
Incidence of Nausea and vomiting was equivalent in both the groups, which was not significant, which could be due to anti emetic action of both dexamethasone and dexmedetomidine. Similar results were observed in a study conducted by Thakur J et al. [16]. Incidence of sedation was found in only 3 patients in group II, which was again not significant compared to group I as we used only 0.5 mcg/kg of dexmedetomidine as an adjunct to ropivacaine.
LIMITATIONS
Limitations include absence of a control group (LA without an adjuvant) to compare the efficacy of adjuvant with control group, inaccurate VAS scores in the first few hours following surgery and the inability to compare the time at which analgesics began to act in different groups because of the persisting effect of SAB.
CONCLUSION
When used in conjunction with ropivacaine, dexmedetomidine and dexamethasone significantly reduced the post-operative pain levels, lengthened the duration of analgesia, reduced the need for rescue analgesia and increased the patient satisfaction with more effective block quality. However, dexmedetomidine modestly outperforms dexamethasone in terms of duration and quality of analgesia, as well as the reduction in the requirement for rescue analgesics.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICT OF INTERESTS
Declared none
REFERENCES
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia. 2011 Jun;15(3):239-49. doi: 10.1007/s10029-011-0798-9, PMID 21365287. PMID 21365287.
Joshi GP, Rawal N, Kehlet H, Prospect Collaboration, Bonnet F, Camu F. Evidence-based management of postoperative pain in adults undergoing open inguinal hernia surgery. Br J Surg. 2012 Feb;99(2):168-85. doi: 10.1002/bjs.7660, PMID 21928388.
Petersen PL, Mathiesen O, Torup H, Dahl JB. The transversus abdominis plane block: a valuable option for postoperative analgesia? a topical review. Acta Anaesthesiol Scand. 2010;54(5):529-35. doi: 10.1111/j.1399-6576.2010.02215.x, PMID 20175754.
Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21(4):325-33. doi: 10.1002/ca.20621, PMID 18428988.
Mishra M, Mishra SP. Transversus abdominis plane block: the new horizon for postoperative analgesia following abdominal surgery. Egypt J Anaesth. 2016 Apr;32(2):243-7. doi: 10.1016/j.egja.2015.12.003.
Sharkey A, Borglum J, Blanco R, McDonnell J. TAP block: past, present and future. Am Soc Reg Anesth Pain Med. 2014;12:15-7.
Gropper MA, Miller RD. Millers anesthesia peripheral nerve blocks and ultrasound guidance for regional anesthesia; Elsevier Health Sciences; 2019 Oct 7. p. 793-825.
Weerink MA, Struys MM, Hannivoort LN, Barends CR, Absalom AR, Colin P. Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine. Clin Pharmacokinet. 2017;56(8):893-913. doi: 10.1007/s40262-017-0507-7, PMID 28105598, PMCID PMC5511603.
Krishna Prasad GV, Khanna S, Jaishree SV. Review of adjuvants to local anesthetics in peripheral nerve blocks: current and future trends. Saudi J Anaesth. 2020;14(1):77-84. doi: 10.4103/sja.SJA_423_19, PMID 31998024, PMCID PMC6970354.
Sinha J, Pokhriyal AS, Asthana V, Nautiyal R. Nautiyal dexmedetomidine vs dexamethasone as an adjuvant to levobupivacaine in ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing total abdominal hysterectomies. Anesthesiol Pain Med. 2023;13(6):e142059. doi: 10.5812/aapm-142059, PMID 38666229.
Aguirre Ospina OD, Gomez Salgado JC, Chaverra D, Alzate M, Rios Medina AM. Bloqueo del plano transverso del abdomen en herniorrafia inguinal. Ensayo clinico controlado. Rev Colomb Anestesiol. 2017;45(3):159-65. doi: 10.1016/j.rca.2017.03.002.
Desmet M, Braems H, Reynvoet M, Plasschaert S, Van Cauwelaert J, Pottel H. I.V. and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: a prospective randomized placebo-controlled study. Br J Anaesth. 2013;111(3):445-52. doi: 10.1093/bja/aet109, PMID 23587875.
Madangopal RM, Dang A, Aggarwal M, Kumar J. A comparative evaluation of different doses of dexmedetomidine as an adjuvant to bupivacaine in transversus abdominis plane block for postoperative analgesia in unilateral inguinal hernioplasty. J Anaesthesiol Clin Pharmacol. 2020 Jul-Sep;36(3):398-406. doi: 10.4103/joacp.JOACP_26_19, PMID 33487910, PMCID PMC7812963.
Zhang P, Liu S, Zhu J, Rao Z, Liu C. Dexamethasone and dexmedetomidine as adjuvants to local anesthetic mixture in intercostal nerve block for thoracoscopic pneumonectomy: a prospective randomized study. Reg Anesth Pain Med. 2019 Aug 8:44(10):100221. doi: 10.1136/rapm-2018-100221, PMID 31399540.
Singla N, Garg K, Jain R, Malhotra A, Singh MR, Grewal A. Analgesic efficacy of dexamethasone versus dexmedetomidine as an adjuvant to ropivacaine in ultrasound-guided transversus abdominis plane block for post-operative pain relief in caesarean section: a prospective randomised controlled study. Indian J Anaesth. 2021;65 Suppl 3:S121-6. doi: 10.4103/ija.IJA_228_21, PMID 34703057, PMCID PMC8500199.
Thakur J, Gupta B, Gupta A, Verma RK, Verma A, Shah P. Aprospective randomized study to compare dexmedetomidine and dexamethasone as an adjunct to bupivacaine in transversus abdominis plane block for post-operative analgesia in caesarean delivery. Int J Reprod Contracept Obstet Gynecol. 2019;8(12):4903-8. doi: 10.18203/2320-1770.ijrcog20195342.
Elhamamy N. Ultrasound-guided transversus abdominis plane block by using bupivacaine alone or when mixed with dexmedetomidine or dexamethazone for pain relief among abdominal hysterectomy patients. JGWH. 2020;18(1). doi: 10.19080/JGWH.2020.18.555979.