
Int J Curr Pharm Res, Vol 17, Issue 5, 86-90Original Article
PERCEPTIONS OF COMPETENCY BASED MEDICAL EDUCATION IMPLEMENTED IN MEDICAL EDUCATION AMONG UNDERGRADUATE MEDICAL STUDENTS IN A TERTIARY CARE TEACHING HOSPITAL IN A DISTRICT OF ASSAM
ALPANA P. RABHA
Department of Community Medicine, FAAMC and H, Barpeta, Assam
*Corresponding author: Alpana P. Rabha; *Email: alporabha@gmail.com
Received: 10 Jun 2025, Revised and Accepted: 30 Jul 2025
ABSTRACT
Objective: Medical education recently reforms the structure, components, time-bound, learner centric new curriculum known as competency based medical education all over the country. Being implemented as a new CBME curriculum in Medical education, the study has been initiated to assess the perception towards CBME among the UG students in a medical college of Assam.
Methods: A cross-sectional study was conducted among Phase 1 UG medical students of 2024-25 batch admitted to FAAMCH, Barpeta Assam. Data were collected by self-administered questionnaire method after taking informed consent for the study. The responses were assessed and analyzed.
Results: A total of 123 students from Phase I MBBS participated in this study. Among them 84 (68.29%) male and 39 (31.71%) were female students, 80 (65.4%) from 20-23 y, 107 (86.99%) from nuclear and 16 (13%) from joint family. Majority of the students 80 (65.04%), 30 (24.39%), 13 (10.56%) belonged to rural, urban and semi-urban area. Awareness about new CBME curriculum 119 (96.74%), 115(93.49%) various domains of TLM, Role of IMG and FAP were 100%; only 71(57.72%) aware about revised guidelines. Knowledge of various components of CBME curriculum was found to be more than 90% except Learner doctor program 76 (61.78%), electives 42 (34.14%), disability guidelines 39(31.7%) and revised CBME guidelines 73 (59.35%).
Conclusion: The study participants perception towards various curricular components were found to be satisfactory. 71.42% of the students having satisfactory, 17.14% having average and 21.42% having poor knowledge on Curricular components of CBME.
Keywords: Curriculum, Competency based medical education, Medical students, Perception
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i5.7056 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Medical education is the process of teaching, learning and training of students with an ongoing integration of knowledge, experience, skills, qualities, responsibility and values which qualify an individual to practice medicine. Recently there has been change in the medical education by replacing old traditional curriculum and introducing CBME, competency based medical education in the undergraduate medical curriculum. The main intention of introduction of CBME was to take the learner to provide health care to the evolving needs of the nation and the world. By Frank., et al.1 in 2010 “ Competency based education (CBE) is an approach to preparing physicians for practice that is fundamentally oriented to graduate outcome abilities and organized around competencies derived from an analysis of societal and patient needs. It de-emphasizes time-based training and promises greater accountability, flexibility, and learner-centeredness”. WHO in 2013 2, also recommended health professional education initiative to produce competent professionals who could carry out not only their duties but also to fulfil health care needs of the people. By Gruppen et al. 5 also highlighted the beneficial role of competency based education in resource poor setting in improving Global health. The new regulation in medical education implemented is more learner centric, patient centric, gender sensitive, outcome orientated and environment appropriate. Being implemented as a new CBME curriculum in Medical education, the study has been initiated to know the perception towards CBME among the UG medical students in a medical college of Assam.
MATERIALS AND METHODS
Study design: A cross-sectional (questionnaire-based) study.
Study place and duration the study: The study was conducted from December 2024-February 2025 in Tertiary care health facility (FAAMCH), Barpeta, Assam.
Sampling method: All the phase I MBBS students of 2024-25 batch have been included for the study. By convenient sampling method 123 students had participated in this study.
Inclusion and exclusion criteria: Those who had given informed consent after explaining to the purpose of the study and was present during the day of survey included for the study. Those who were absent on the day of survey were excluded from the study.
Ethical committee approval was obtained before initiation of the study with ref No: FAAMC and H/P. Est/IEC/26/Pt-1/2022/104.
Procedure
The study was carried out after getting the approval from the Institutional Ethics Committee. The data were collected by questionnaire method. The questionnaire consisting of 1) Socio-demographic profile of the study participants, 2) Awareness of CBME, 3) Knowledge and perception of various components of CBME curriculum, 4) Attitudes towards CBME curriculum. Options of questions were framed “Yes”/“no” and attitudes responses “agree”, “disagree”, “neutral”, “strongly agree “ and “strongly disagree”
Statistical analysis
The data were entered Microsoft excel sheet with coding and analysis were expressed in frequency, percentages and with diagrammatic representations.
RESULTS
The present study was conducted among 123 Phase 1 (first year MBBS) students in a medical college of Assam. Out of 123 students 84 (68.29%) male, 39 (31.71%) female, 80 (65.4%) belonged to 20-23 y, 80 (65.04%) from rural, 30 (24.39%) urban and 13 (10.6%) semi-urban, 107 (86.99%) nuclear and 16 (13%) living in joint family.
Table 1 showing the socio-demographic profile of the study participants.
Table 2 Most of the participants 119 (96.74%) were aware about the new curriculum, 115 (93.49%) about CBME as outcome based with various domains of TLM and assessment, 123 (100%) about role of IMG and FAP, but only 71 (57.72%) about revised guidelines and 22 (17.88%) about GMER 23.
Table 3 Shows the knowledge on FAP was found to be 100 (81.3%), core elements of CBME 120 (97.56%), TLM 116 (94%), goal of CBME 104 (84.5%), mentor-mentee program 120 (97.56%), FC 108 (87.80%), course duration 112 (99.18%), assessment tool 108 (87.80%), revised passing criteria 122 (99.18%), eligibility for appearing professional examination 112 (91.05%); but learner doctor programme 76 (61.78%), electives 42 (34.14%) and revised CBME guidelines 73 (59,35%).
Table 4 shows about various Teaching learning methods perceived by the participants. Around 105 (85.37%) knows about all the various TLM, preferences on group discussion (G D) 80 (65.04%), 14 (11.38%) on SGT; 5 (4.06%) on SDL; more effective method perceived as SGT (22.76%), Seminar 27 (21.95%), tutorials 20 (16.26%), SDL 22 (17.88%), Lecture 7 (5.69%) by the study participants.
Table 1: Socio-demographic profile of the study participants
| Variables | Age | Frequency | Percentage |
| Age distribution | 17-19 20-23 24-27 |
19 80 4 |
31.71% 65.4% 3.25% |
| Sex | Female Male |
39 84 |
31.71% 68.29% |
| Caste | General OBC ST(H) ST(P) SC |
58 35 7 10 13 |
47.15% 28.46% 5.69% 8.13% 10.57% |
| Religion | Hindu Muslim Christian Buddhist |
72 48 2 1 |
58.54% 39.02% 1.63% 0.81% |
| Residence | Rural Urban Semi-urban |
80 30 13 |
65.04% 24.39% 10.56% |
| Type of family | Nuclear Joint |
107 16 |
86.99% 13% |
| Income (monthly) | <60,000/ 1,00,000/-1,50,000/ 1,50,000/-2,00,000/ >2,00,000/ |
65 32 14 12 |
52.84% 26.01% 11.38% 9.75% |
Table 2: Responses showing awareness of CBME among the study participants
| Variables | Yes (%) (N 123) | No (%) |
| Are you aware on new curriculum in Medical education? | 119 (96.74%) | 4 (3.25%) |
What is CBME – Outcome based where various domains of TLM and Assessment framework of competencies? |
115 (93.49%) | 8 (6.5%) |
| Role of IMG | 123 (100%) | 0 |
| Do you know about GMER 2023? | 22 (17.88%) | 101 (82.11%) |
| Are you aware about revised CBME guidelines? | 71 (57.72%) | 52 (42.27%) |
| What are dimensions of competency? – attitudes/knowledge/skills/behaviour/all | 85 (69.10%) | 38 (30.89%) |
| Awareness about FAP | 123 (100%) | 0 |
Table 3: Knowledge on components of competency based medical education curriculum
| Knowledge on components of CBME curriculum | Yes (%) (N =123) | No (%) |
|
100(81.3%) | 23(18.69%) |
|
120(97.56%) | 3(2.4%) |
|
116(94%) | 7(5.6%) |
|
104(84.5%) | 19(15.44%) |
|
76(61.78%) | 47(38.21%) |
|
39(31.7%) | 84(68.29%) |
|
120(97.56%) | 3(2.4%) |
|
42(34.14%) | 81(65.85%) |
|
108(87.80%) | 15(12.19%) |
|
112(91.05%) | 11(8.94%) |
|
122(99.18%) | 1(0.81%) |
|
108(87.80%) | 15(12.19%) |
|
112 (99.18%) | 1(0.81%) |
|
73 (59.35%) | 50(40.65%) |
Table 4: Responses showing teaching learning methods on CBME among study participants
| Questions | Responses | Frequency, N (123) | Percentage (%) |
|
SGT/SGD/l/PEDOGOGY/CORRELATION/ INTEGRATED SEMINAR/ALL SGT/SGD/IS/l No responses |
105 08 10 |
85.37% 6.5% 8.13% |
Prefer as students? |
Small Group Teaching (SGT) Self Directed Learning (SDL) Integrated Seminar (IS) Group Discussion (GD) ALL(SDL/GD/l/Q/A/IS) |
14 05 05 80 19 |
11.38% 4.06% 4.06% 65.04% 15.44% |
|
L(Lecture) SGT TU(Tutorial) SEMINAR SDL ALL(L/SDL/SGT/GD/IS/TU) Total |
7 28 20 27 22 19 123 |
5.69% 22.76% 16.26% 21.95% 17.88% 15.44% |
Table 5: Attitude based responses on CBME curriculum among the study participants
| Questions related to CBME curriculum | Responses | Frequency | Percentage (%) |
| Q1 Do you think CBME – good effect on quality of Medical education? | Yes | 123 | 100% |
| Q2 What is your opinion about FC in curriculum ? Is it necessary for CBME curriculum? | Yes | 123 | 100% |
| Q3 CBME encourages learners to reflect on their performances and take responsibility for their own learning and professional development | Agree Disagree Neutral Strongly agree |
89 1 18 15 |
72.36% 0.81% 14.63% 12.20% |
| Q4 Do you think all types of TM helpful for the students/teachers? | Yes No |
83 20 |
67.48% 32.52% |
| Q5 Do you think CBME curriculum is student/teacher centric/both? | Student centric Teacher centric Both |
3 12 107 |
2.44% 9.76% 86.99% |
| Q6 Do you think that introduction of AETCOM module will help in improving the communication skills? | Agree Neutral Strongly agree |
95 3 24 |
77.24% 2.44% 19.51% |
| Q 7 Do you think that all applied TM in CBME curriculum needed infrastructure facilities? | Yes No |
105 18 |
85.36% 14.64% |
| Q 8 Do you think that CBME has many dimensions in learning process? | Yes No |
118 5 |
95.93% 4.07% |
| Q 9 Do you think CBME curriculum more stressful than traditional medical education? | Agree Disagree Neutral Strongly agree Strongly disagree |
35 25 49 8 5 |
28.46% 20.33% 39.84% 6.50% 4.07% |
| Q10 Do you think Yoga and meditation, sports and extracurricular activities important in CBME curriculum? | Agree Neutral Strongly agree Strongly disagree |
72 3 44 1 |
58.54% 2.44% 35.77% 0.81% |
| Q11 Do you think feedback, logbook and record (case-based) important inputs of CBME curriculum? | Agree Disagree Neutral Strongly agree |
87 4 17 14 |
70.73% 3.25% 13.82% 11.38% |
| Q12 Do you think CBME curriculum will help in preparation of NeXT? | Yes No |
117 6 |
95.12% 4.88% |
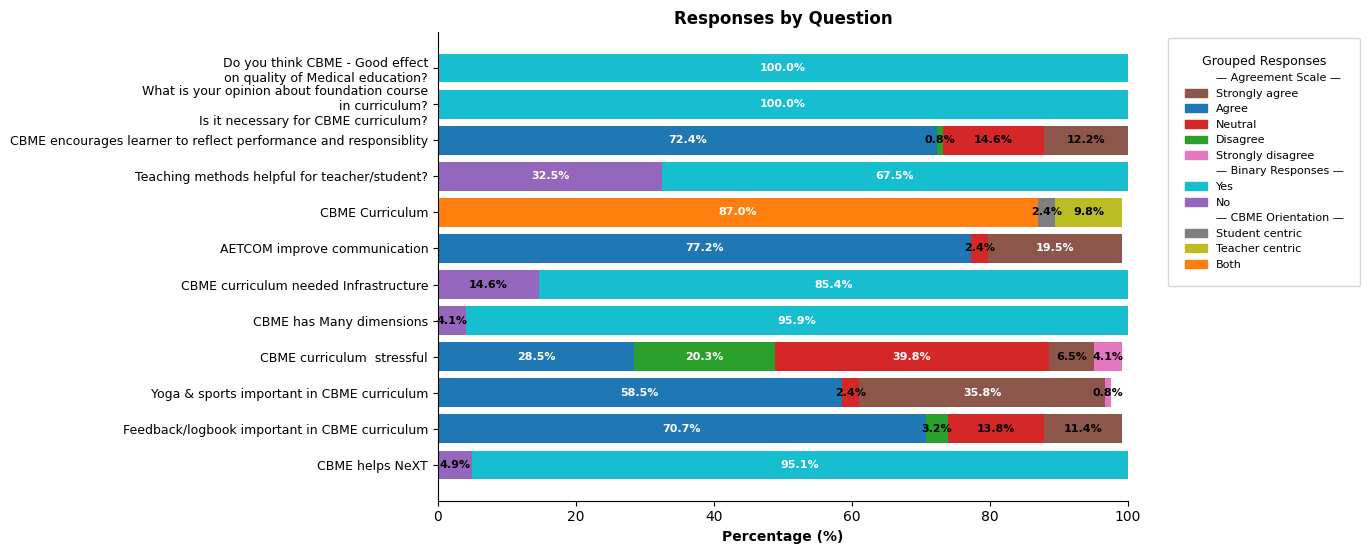
Fig. 1: Showing responses to attitude based questions on CBME curriculum among the study participants
Fig. 1 showed most of the participants 123 (100%) were positively responded CBME as good effect on quality of medical education and also 100% responded about foundation course. 95% of students were positively responded on AETCOM module in improving the communication skills. Around 35 (28.46%) agreed that CBME curriculum more stressful than traditional method. The need for yoga and meditation, sports and extracurricular activities, 44 (35.77%) strongly agreed, 72 (58.54%) agreed, only 3 (2.44%) responded as neutral. Logbook, feedback and record based preferences were 87 (70.73%), strongly agreed 14 (11.38%).
Fig. 2 showed that 111 (90.24%) students were given positive responses about the strength of CBME as course timeline, time distribution of each phase of MBBS curriculum, eligibility to appear and passing criteria for university examination, assessment and progression, teaching learning experiences.
Table 6: Showing responses on strength of CBME curriculum
| What are the strength of CBME curriculum? | Frequency | Percentages (%) |
| 1)MBBS course timelines | 1 | 0.81% |
| 2)Time distribution of each phase of MBBS curriculum | 1 | 0.81% |
| 3)eligibility to appear and passing criteria for university examination | 4 | 3.25% |
| 4) Assessment and progression | 2 | 1.63% |
| 5) Teaching learning experiences | 1 | 0.81% |
| 6) All of the above statement | 111 | 90.24% |
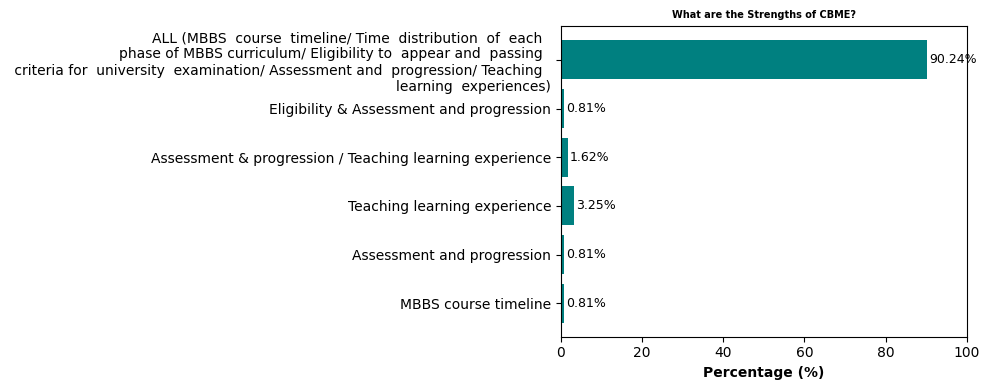
Fig. 2: Showing responses on strength of CBME curriculum
Table 7: Showing responses of study participants on family adoption programme
| Questions related to family adoption programme | Responses | Frequency | Percentage (%) |
| Do you aware about Family adoption programme in CBME curriculum? | Yes | 123 | 100% |
| If yes, then how many visit allotted as per CBME curriculum during Phase I MBBS course. | No visit 6 7 8 9 |
23 32 21 19 28 |
18.70% 26.02% 17.07% 15.45% 22.76% |
| FAP offers medical students – new experimental learning opportunity/research? | Yes No |
122 1 |
99.19% 0.81% |
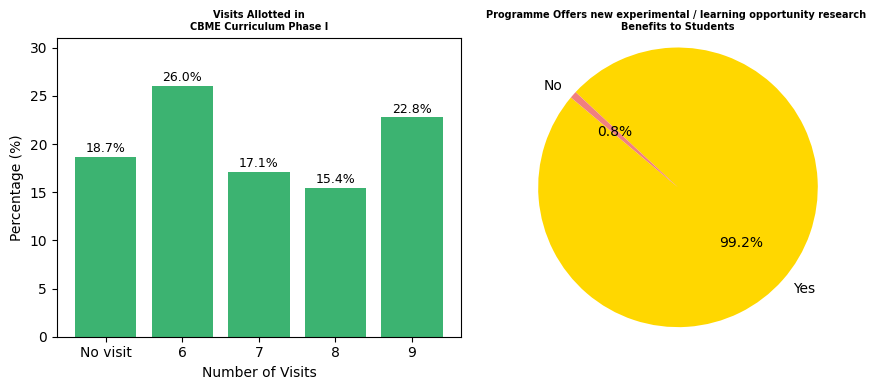
Fig. 3: Showing responses on FAP among study participants
Family visits as part of family adoption programme, majority 123 (100%) were aware about the FAP and 122 (99.19%) gave positive responses as new experimental learning opportunities/research; whereas only 28 (22.76%) had correctly answered on number of visits during first (phase I) year of MBBS course.
DISCUSSION
The present study was conducted among 126 Phase I (first year) MBBS students in a Medical college of Assam regarding perceptions of the various components of Competency Based Medical Education curriculum. Out of 126,123 undergraduate first year medical students were participated in this study.
Among the 123 students, 119 (96.74%) were aware about the new CBME curriculum whereas in a study done by P Selva 6 revealed only 17.1% not even aware about new curriculum. Awareness of CBME as outcome based with various Teaching Learning Methods (TLM) 116 (94%),123 (100%) about role of Indian Medical Graduate (IMG) and Family Adoption Programme (FAP) except 71 (57.72%) aware about revised guidelines; 22 (17.88%) about GMER 2023.
Knowledge on various components of CBME curriculum such as core elements was 120 (97.56%), TLM 116 (96%), mentor-mentee program 120 (97.56%), FC 108 (87.80%), tools of assessment 108 (89.80%), course duration 112 (99.18%), only 76 (61.78%) on learner-doctor program, electives 42 (34.14%). The perceived preference of TLM among the students was found to be group discussion 80 (65.04%), followed by SGT 14(11.38%), SDL 5 (4.06%), IS 5(4.06%), and all 11 (15.44%). But by Shanmathi KA7 mentioned SGT received high approval from 83.7% of students in their study. In CBME, perceived most effective TLM as SGT 28 (22.76%), Seminar 27 (21.95%), SDL 22 (17.88%), Tutorial 20 (16.26%), only 7 (5.69%) as Lecture and all methods 17(13.82%); whereas by Majeed M et al. 8 found 35% agreed that SDL should be incorporated in the curriculum in their study. Ramanathan R et al.9 in their study, also revealed that SDL and reflective learning were not appreciated by the students and similarly by Sharma S et al. [10] also found SDL received the lowest positive responses (57-58%). The present study found that the students also perceived tracking about their progression of learning experiences through academic mentor 75 (60.98%), department 33 (26.83%), academic cell 8 (6.50%). All the participants 123 (100%) responded CBME as good effect on quality of medical education and also on Foundation course. Around 89 (72.36%) agreed CBME encourages learners to reflect their performances, strongly agreed 15 (12.20%), disagreed only 1(0.81%). Similar study done by Shetty AK et al. [11] also mentioned positive responses to the usefulness of various components of CBME. All types of teaching methods applied in CBME, responded by the participants helpful for teacher and student 107 (86.99%), AETCOM module 95 (77.24%) agreed helpful in communication skills. Infrastructure facilities identified important in CBME curriculum by the respondent positively 105 (85.36%). Majority 118 (95.93%) responded as CBME has many dimensions in learning process. 35 (28.46%) agreed, 25 (20.33%) disagreed, 49 (39.84%) neutral on CBME curriculum more stressful than traditional medical education. In a study done by Li Ai Erica et al. [12] also found to be more positive about the CBME curriculum among the students. Regarding Yoga and meditation, sports and extracurricular activities, 72 (58.54%) agreed, 44 (35.77%) strongly agreed by the participants. Logbook, feedback and record (case based) components of CBME curriculum, 87 (70.73%) agreed, 17 (13.82%) neutral, 14 (11.38%) strongly agreed among the participants. CBME curriculum helpful in preparation of Next responded 117 (95.12%) by the participants.
CONCLUSION
The study concluded that the awareness, knowledge, attitude and perceptions towards competency based medical educations among medical students was satisfactory. The CBME curriculum makes the various learning methods more relevant, understanding to the students. The new CBME curriculum may improve the delivery and tracking of progression of learning experiences both for faculties as well as to the students in future.
LIMITATION OF THE STUDY
The present study has been conducted in a medical college with a smaller number of participants. The findings could not be generalized to larger group.
ETHICAL APPROVAL
The study was approved by the Institutional Ethics Committee.
FUNDING
Nil
ACKNOWLEDGEMENT
The author would like to thank all the students who had participated for successful completion of the study.
CONFLICT OF INTERESTS
Declared none
REFERENCES
Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR. Competency based medical education: theory to practice. Med Teach. 2010;32(8):638-45. doi: 10.3109/0142159X.2010.501190, PMID 20662574.
Health manpower development. WHO Chron. 1976;30(1):32-4. PMID 1246876.
Medical Council of India. Graduate Medical Education Regulations, 1997. No. MCI-34(41)/Med/161726; amended 2019. New Delhi: Medical Council of India; 2019.
NMC (UGMEB). Implementation of new competency based medical education for UG course curriculum/no U11016/I/2022-UGMEB; 2023 Mar 31.
Gruppen L, Frank JR, Lockyer J, Ross S, Bould MD, Harris P. Toward a research agenda for competency based medical education. Med Teach. 2017;39(6):623-30. doi: 10.1080/0142159X.2017.1315065, PMID 28598741.
Selva P, Rithika M. Perspectives of students and teaching faculty members. Towards the new MBBS curriculum in a Tertiary Care Hospital in Chennai. Int J Curr Res Rev. 2021 Apr;13(8):120-6. doi: 10.31782/IJCRR.2021.13810.
Shanmathi KA, Meena TS, Selvam V, Revathy TG. Assessing the impact of competency based medical education (CBME): insights from medical students Texila. Int J Pub Health. 2013;12(4):Art023. doi: 10.21522/TIJPH.2013.12.04.Art023.
Majeed M, Ashraf Z, Manzoor S, Bashir S. Understanding the perception of medical students regarding the newly introduced competency based medical education and identifying the challenges which hamper its proper implementation. JK Pract. 2023;28(1-2):35-41.
Ramanathan R, Shanmugam J, Gopalakrishna SM, Palanisami K, Narayanan S. Exploring the learners perspectives on competency based medical education. J Educ Health Promot. 2021 Mar 31;10:109. doi: 10.4103/jehp.jehp_866_20, PMID 34084856.
Sharma S, Chhatwal J. Perspectives of undergraduate medical students regarding competency based curriculum. Natl Med J India. 2023;36(6):379-83. doi: 10.25259/NMJI_461_2022, PMID 38909299.
Shetty AK, Sarala N, Geetha S, Shankar MS. Perception of competency based medical education curriculum: insights from three batches. Int J Acad Med. 2024;10(3):103-8. doi: 10.4103/ijam.ijam_58_23.
Ai Li E, Wilson CA, Davidson J, Kwong A, Kirpalani A, Wang PZ. Exploring perceptions of competency based medical education in undergraduate medical students and faculty: a program evaluation. Adv Med Educ Pract. 2023;14:381-9. doi: 10.2147/AMEP.S399851, PMID 37101694.