
Int J Curr Pharm Res, Vol 17, Issue 5, 99-102Original Article
SONOGRAPHIC ASSESSMENT OF VARIOUS THYROID NODULES AND THEIR CORRELATION TO HISTOPATHOLOGICAL EXAMINATION
RAMARAPPU SOWMYA*, VULCHI HEMANTH, VATTIGUNTA NIRUPAMA
Department of Otorhinolaryngology, Dr. Patnam Mahender Reddy Institute of Medical Sciences, Chevella, Rangareddy-501503, Telanana, India
*Corresponding author: Ramarappu Sowmya; *Email: s.ramarappu@gmail.com
Received: 11 Jun 2025, Revised and Accepted: 01 Aug 2025
ABSTRACT
Objective: High-resolution ultrasonography (USG) and fine-needle aspiration cytology (FNAC) are cornerstone tools for initial evaluation, while histopathological examination (HPE) serves as the definitive diagnostic method. This study is to compare the efficacy of both these methods in the diagnosis of thyroid nodules.
Methods: This prospective cross-sectional study included 100 patients with thyroid nodules evaluated at a tertiary care center over 18 mo. Each patient underwent USG, FNAC, and subsequent surgical histopathology when indicated. Sonographic features such as echogenicity, margin irregularity, calcifications, shape, and vascularity were assessed. Nodules were classified using TI-RADS and FNAC results interpreted using the Bethesda system. Final histopathology served as the gold standard.
Results: The study population was predominantly female (75%), with an average age of 42.6 years. Solitary nodules were more common (72%), primarily affecting the right lobe. Sonographic features such as hypoechogenicity, irregular margins, microcalcifications, taller-than-wide shape, and increased central vascularity were significantly associated with malignancy (p<0.05). Higher TI-RADS (4 and 5) and Bethesda categories (V and VI) strongly correlated with malignant histopathology (p<0.0001). A rising trend in malignancy risk was observed with ascending TI-RADS and Bethesda scores.
Conclusion: This study reaffirms the diagnostic value of USG and FNAC in thyroid nodule evaluation. Significant correlation between TI-RADS and Bethesda classifications with histopathological outcomes underscores their complementary role in malignancy risk stratification and clinical decision-making.
Keywords: Thyroid nodules, Ultrasound, Fine needle aspiration cytology
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i5.7061 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Thyroid nodules are separate lesions located in the thyroid gland that appear different from the adjacent parenchyma on imaging studies [1]. They are frequently observed in clinical settings, with a prevalence that rises with age and exposure to risk factors like radiation and iodine lack. Although the majority of thyroid nodules are benign and show no symptoms, a small fraction could be malignant, highlighting the importance of precise diagnosis. These nodules can appear as noticeable lumps, can be found during imaging, or lead to compressive symptoms or hormonal disturbances based on their size and activity.
Assessment of thyroid nodules usually starts with a detailed clinical evaluation, followed by an ultrasound examination. Sonographic assessment plays a crucial role in the initial evaluation and risk stratification of thyroid nodules. High-resolution ultrasound is the preferred imaging technique, offering precise details regarding the nodule’s size, composition (solid, cystic, or mixed), echogenicity, margins, calcifications, and blood flow [1]. Color Doppler imaging is frequently utilized in conjunction with grayscale ultrasound to evaluate intranodular and perinodular blood flow, assisting in distinguishing between benign and malignant nodules. Utilizing these characteristics, nodules can be classified through established systems such as the Thyroid Imaging Reporting and Data System (TI-RADS), which directs subsequent diagnostic procedures like fine-needle aspiration cytology (FNAC).
The occurrence of nodules rises with age and is more prevalent in women, individuals with iodine deficiency, and those exposed to radiation. The global prevalence of thyroid nodules in the general population has been estimated to exceed 67%, varying based on detection method (palpation, ultrasound, or autopsy) and significantly differing by country [2, 3]. Various research indicates a prevalence of 2-6% through palpation, 19-35% via ultrasound, and 8-65% according to autopsy findings [4, 5]. Ultrasonography exhibits greater sensitivity than palpation, identifying nodules of any size in as many as 67% of the general population [4]. Recent studies indicate that the prevalence of thyroid nodules in India is 12.2%, while the incidence of thyroid cancers is significantly lower, around 8.7 per 100,000 individuals [6, 7].
Integrating ultrasound results with histopathological examination continues to be essential for assessing the characteristics of thyroid nodules and developing suitable treatment plans. FNAC is a commonly employed minimally invasive procedure for the initial assessment of thyroid nodules and has a strong correlation with histopathological examination (HPE), which is the conclusive diagnostic approach. Although FNAC is very precise in detecting benign and malignant lesions, histopathology assists in verifying these results and elucidating ambiguous or inconclusive cytological findings. Additionally, USG and FNAC work together effectively, with ultrasound aiding in the choice of nodules for aspiration and improving diagnostic outcomes, particularly when paired with standardized scoring systems such as TI-RADS and Bethesda.
This study aimed to assess thyroid nodules through high-resolution ultrasonography and fine-needle aspiration cytology (FNAC), and to link these results with final histopathological analysis. The objective was to evaluate the diagnostic precision and agreement among sonographic, cytological, and histopathological characteristics.
MATERIALS AND METHODS
Study design
This was a prospective cross-sectional study conducted over a period of 18 mo in the Department of Otorhinolaryngology in collaboration with the Department of Pathology and Radiology at a tertiary hospital in Chevella, Telangana, India.
Study population
A total of 100 patients presenting with thyroid nodules, either palpable or incidentally detected on imaging, were recruited for the study. All participants underwent ultrasound evaluation followed by fine needle aspiration cytology (FNAC) and, when indicated, histopathological examination post-thyroidectomy.
Inclusion criteria
Adults aged 18 to 70 y
Patients with palpable thyroid nodules
Patients with incidentally detected thyroid nodules on imaging
Patients undergoing both USG and FNAC followed by surgery
Exclusion criteria
Patients with a previous history of thyroid malignancy.
Individuals who had undergone prior thyroid surgery.
Pregnancy.
Present or old history of chemoradiation.
Patients unwilling to undergo FNAC or surgery if indicated.
Data assessment
Every patient enrolled underwent:
Clinical assessment, comprising a thorough history and physical examination.
Thyroid Function Tests.
Ultrasonography with high resolution utilizing a 7.5–12 MHz linear probe for evaluation:
Nodule dimensions
Form (broader-than-high vs. higher-than-broad)
Echogenicity (hypoechoic, isoechoic, hyperechoic)
Borders (smooth, uneven, microlobulated)
Existence of calcified deposits (micro or macro)
Internal structures (solid, cystic, complex)
Vascularity (central, peripheral, combined)
Nodules were classified based on TI-RADS for evaluating the risk of malignancy.
All patients received ultrasound-guided FNAC, and the samples were classified according to the Bethesda System for Reporting Thyroid Cytopathology (BSRTC).
Histopathological evaluation
Removed thyroid tissues were preserved in 10% formalin, sliced, and stained with Hematoxylin and Eosin (H and E) for microscopic analysis.
Final diagnoses were categorized as benign (e. g., colloid goiter, adenoma) or malignant (e.g., papillary carcinoma, follicular carcinoma) according to WHO guidelines.
Statistical analysis
All gathered data were inputted and compiled using Microsoft Excel and assessed with SPSS software version 25.0. Means, standard deviations, and percentages were computed to summarize demographic information and sonographic characteristics. Connections between specific sonographic features (including echogenicity, margins, calcifications, and vascularity), FNAC to final histopathological results were examined using the Chi-square test or Fisher’s exact test as suitable. A p-value under 0.05 was considered as statistically significant.
OBSERVATIONS AND RESULTS
Table 1 shows the demographic characteristics of the study group, with an average age of 42.6 y and a majority of females (75%). The majority of patients had individual thyroid nodules, with the right lobe being the most frequently affected area.
Table 1: Demographic characteristics of the study population (n = 100)
| Parameter | Mean±SD/n (%) |
| Age (years) | 42.6±12.3 |
| Gender (Female: Male) | 75:25 (3:1) |
| Type of Nodule | |
| – Solitary | 72 (72%) |
| – Multiple | 28 (28%) |
| Lobe Involvement | |
| – Right | 58 (58%) |
| – Left | 34 (34%) |
| – Isthmus | 8 (8%) |
Table 2 illustrates the distribution of important ultrasound characteristics among benign and malignant nodules. Characteristics like hypoechogenicity, uneven borders, microcalcifications, and a taller-than-wide appearance were strongly linked to malignancy (p<0.05).
Table 2: Distribution of ultrasonographic features in thyroid nodules
| Sonographic feature | Benign (n = 74) | Malignant (n = 26) | p-value |
| Hypoechogenicity | 24 | 18 | 0.0007 |
| Irregular Margins | 16 | 14 | 0.0004 |
| Microcalcifications | 8 | 10 | 0.00001 |
| Taller-than-wide Shape | 6 | 12 | 0.0001 |
| Increased Central Vascularity | 12 | 14 | 0.0003 |
Table 3 and fig. 1 shows the distribution of nodules classified by TI-RADS categories and their corresponding final histopathology. A greater TI-RADS score (TI-RADS 4 and 5) was strongly linked to a higher risk of malignancy, showing a statistically significant relationship of p-value<0.0001.
Table 3: Distribution based on TI-RADS categories and final histopathology
| TI-RADS category | Total HPE (n) | Benign HPE(n) | Malignant HPE (n) | p-value |
| TI-RADS 2 | 20 | 20 | 0 | <0.0001 |
| TI-RADS 3 | 28 | 27 | 1 | |
| TI-RADS 4 | 32 | 21 | 11 | |
| TI-RADS 5 | 20 | 6 | 14 |
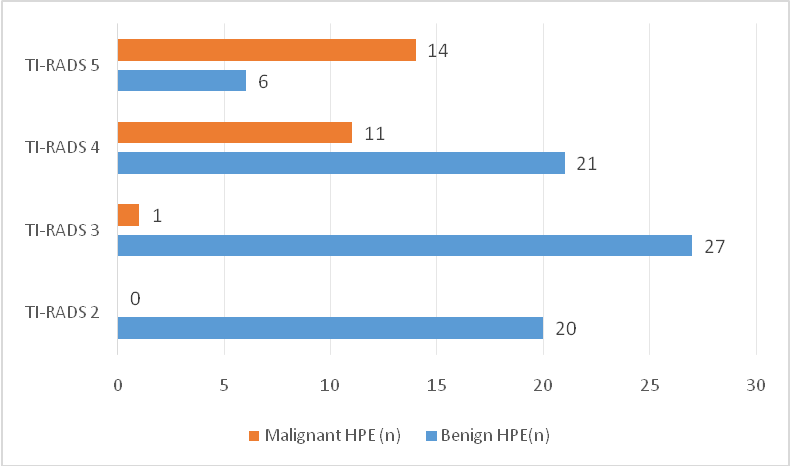
Fig. 1: TI-RADS categories vs histopathological outcome
Table 4: FNAC (Bethesda classification) versus histopathology
| Bethesda category | Total on HPE (n) | Benign on HPE | Malignant on HPE | p-value |
| II (Benign) | 64 | 62 | 2 | <0.0001 |
| III (AUS/FLUS) | 10 | 6 | 4 | |
| IV (Follicular Neoplasm) | 8 | 4 | 4 | |
| V (Suspicious for Malignancy) | 10 | 2 | 8 | |
| VI (Malignant) | 8 | 0 | 8 |
Table 4 and fig. 2 shows the distribution of nodules classified by FNAC categories and their corresponding final histopathology. A greater Bethesda score (V and VI) was strongly linked to a higher risk of malignancy, showing a statistically significant relationship of p-value<0.0001.
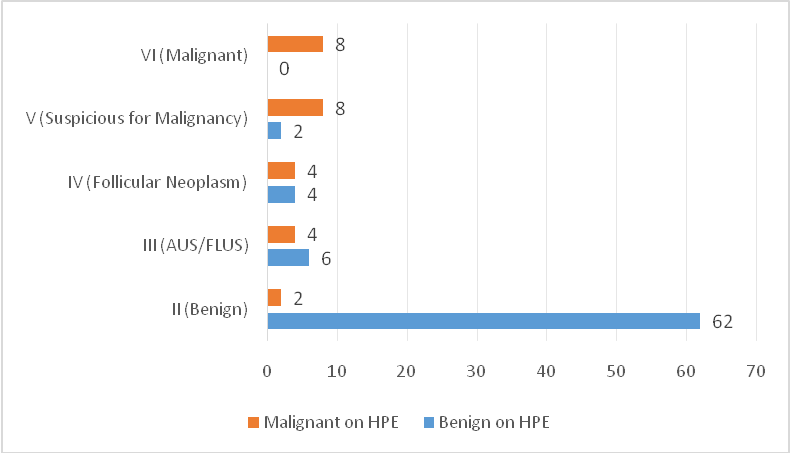
Fig. 2: Bethesda categories vs histopathological outcome
Table 5: Comparison of USG (TI-RADS) categories and FNAC (Bethesda system)
| TI-RADS category | Total nodules (n) | Bethesda II (Benign) | Bethesda III–IV (indeterminate) | Bethesda V–VI (suspicious/malignant) | p-value |
| TI-RADS 2 | 20 | 20 | 0 | 0 | <0.0001 |
| TI-RADS 3 | 28 | 27 | 1 | 0 | |
| TI-RADS 4 | 32 | 17 | 9 | 6 | |
| TI-RADS 5 | 20 | 0 | 2 | 18 |
Table 5 shows that as the TI-RADS category increases, the probability of malignancy in FNAC also rises. TI-RADS 2 and 3 were mainly linked to benign cytology (Bethesda II), whereas TI-RADS 5 demonstrated a significant association with malignant cytology (Bethesda V–VI). This trend showed statistical significance, with a p-value<0.001.
DISCUSSION
The present study involved 100 patients with thyroid nodules, showing an average age of 42.6 y and a significant female majority (75%). The majority of nodules in present study were solitary (72%) and most commonly found in the right thyroid lobe (58%) This demographic trend aligns well with the study done by Isse HM et al. in 2023 [9], where majority of the participants in their study were found to be Female (90%) and 54.7% of the thyroid nodules were found to be solitary.
In this study involving 100 thyroid nodules, various ultrasound characteristics showed a significant correlation with malignancy, with a p-value<0.05. Hypoechogenicity was observed in 69.2% of malignant nodules compared to 32.4% of benign nodules, while irregular margins were found in 53.8% of malignant nodules versus 21.6% of benign ones. Microcalcifications were observed in 38.4% of cancerous nodules, while just 10.8% of non-cancerous ones displayed them. In the same way, a shape that is taller than it is wide (46.1% vs. 8.1%) and central vascularity (53.8% vs. 16.2%) were considerably more frequent in malignant lesions. In comparison to the study conducted by Obad Kovacevic et al. in 2007 [10], the results aligns closely with our study. Their study showed irregular margins and the occurrence of microcalcifications were significantly indicative of cancer, with irregular margins found in 72% of cancerous nodules compared to 18% of non-cancerous ones, and microcalcifications present in 61% of cancerous nodules (p<0.01 for both). Their results additionally discovered that all malignant nodules were devoid of a hypoechoic rim, thus strengthening the diagnostic importance of specific sonographic characteristics. Although heterogeneous echotexture did not exhibit statistical significance in their study, it was not directly evaluated in the present study.
Our results showed a significant relationship between TI-RADS categories and histopathological results. Every nodule categorized as TI-RADS 2 was found to be histologically benign, and only 1 of the 28 TI-RADS 3 nodules was malignant. The occurrence of malignancy was notably higher in elevated TI-RADS categories—34.3% in TI-RADS 4 and 70% in TI-RADS 5 nodules. This clearly indicates that the probability of malignancy rises with increased TI-RADS scores, a correlation that was statistically significant (p<0.0001), strengthening the dependability of TI-RADS in risk assessment. In comparison of our findings with the study conducted by Singaporewalla et al. in 2017 [11]. both revealed a significant link between elevated TI-RADS categories and a greater probability of malignancy. Our results showed 70% of TI-RADS 5 nodules were Malignant, which is closely matching with Singapore Walla’s finding of 60% malignant cases in TI-RADS 5. Similarly, TI-RADS 2 nodules exhibited 100% benign cytology in both the studies.
In comparing our findings with those of Bahaj AS et al. (2020) [12], both studies exhibit a statistically significant correlation between FNAC and ultimate histopathological results (p<0.001). Our results showed that Bethesda II nodules exhibited a 96.9% benign association, which closely matches the findings of Bahaj et al., where 86.2% of Bethesda II nodules were found to be histologically benign. In our study, Bethesda V and VI nodules showed malignancy rates of 80% and 100%, similar to Bahaj's results of 94.5% and 100%, respectively. Both studies affirm that Bethesda categories V and VI are indicative of malignancy.
Our study revealed that 90% (18/20) of TI-RADS 5 nodules were classified as Bethesda V–VI, suggesting a high likelihood or confirmed malignancy, while George et al. in his study in 2022 [13], noted that 97.1% of TI-RADS 5 nodules were malignant on final histopathology, achieving a diagnostic accuracy of 85.7%. Both studies affirm the importance of TI-RADS 5 as a high-risk category, showing a statistically significant link to malignancy (p-value<0.05). Both studies emphasize the practical benefits of combining TI-RADS and Bethesda systems for precise malignancy risk assessment and management strategies in thyroid nodules.
CONCLUSION
This study emphasizes the diagnostic importance of high-resolution ultrasonography and FNAC in assessing thyroid nodules. Ultrasound characteristics like hypoechogenicity, irregular borders, and microcalcifications exhibited a strong association with cancer. Both the TI-RADS and Bethesda classification systems showed a statistically significant correlation with the final histopathology results. Combining these modalities improves precision in risk assessment and directs the best management of thyroid nodules.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
CONFLICT OF INTERESTS
Declared none
REFERENCES
Zamora EA, Khare S, Cassaro S. Thyroid nodule. In: Treasure Island, FL: StatPearls; 2025.
Tan GH, Gharib H. Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med. 1997 Feb 1;126(3):226-31. doi: 10.7326/0003-4819-126-3-199702010-00009, PMID 9027275.
Tran NQ, Le BH, Hoang CK, Nguyen HT, Thai TT. Prevalence of thyroid nodules and associated clinical characteristics: findings from a large sample of people undergoing health checkups at a university hospital in Vietnam. Risk Manag Healthc Policy. 2023;16:899-907. doi: 10.2147/RMHP.S410964, PMID 37220482.
Dean DS, Gharib H. Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab. 2008 Dec;22(6):901-11. doi: 10.1016/j.beem.2008.09.019, PMID 19041821.
Tamhane S, Gharib H. Thyroid nodule update on diagnosis and management. Clin Diabetes Endocrinol. 2016 Oct 3;2:17. doi: 10.1186/s40842-016-0035-7, PMID 28702251.
Bomeli SR, Le Beau SO, Ferris RL. Evaluation of a thyroid nodule. Otolaryngol Clin North Am. 2010 Apr;43(2):229-38. doi: 10.1016/j.otc.2010.01.002, PMID 20510711.
Unnikrishnan AG, Kalra S, Baruah M, Nair G, Nair V, Bantwal G. Endocrine society of India management guidelines for patients with thyroid nodules: a position statement. Indian J Endocrinol Metab. 2011 Jan;15(1):2-8. doi: 10.4103/2230-8210.77566, PMID 21584159.
Chandana DA, Gomathi R, Prakashiny S. Epidemiological and histopathological study of thyroid lesions in a Tertiary Care Hospital in South India. Trop J Pathol Microbiol. 2020;6(6):381-6. doi: 10.17511/jopm.2020.i06.03.
Isse HM, Lukande R, Sereke SG, Odubu FJ, Nassanga R, Bugeza S. Correlation of the ultrasound thyroid imaging reporting and data system with cytology findings among patients in Uganda. Thyroid Res. 2023 Sep 1;16(1):26. doi: 10.1186/s13044-023-00169-1, PMID 37653537.
Kovacevic DO, Skurla MS. Sonographic diagnosis of thyroid nodules: correlation with the results of sonographically guided fine needle aspiration biopsy. J Clin Ultrasound. 2007 Feb;35(2):63-7. doi: 10.1002/jcu.20287, PMID 17206727.
Singaporewalla RM, Hwee J, Lang TU, Desai V. Clinico-pathological correlation of thyroid nodule ultrasound and cytology using the TIRADS and Bethesda classifications. World J Surg. 2017 Jul;41(7):1807-11. doi: 10.1007/s00268-017-3919-5, PMID 28251273.
Bahaj AS, Alkaff HH, Melebari BN, Melebari AN, Sayed SI, Mujtaba SS. Role of fine needle aspiration cytology in evaluating thyroid nodules. A retrospective study from a tertiary care center of Western region, Saudi Arabia. Saudi Med J. 2020 Oct;41(10):1098-103. doi: 10.15537/smj.2020.10.25417, PMID 33026051.
George NA, Suresh S, Jiji V, Renu S, Thomas S, Janardhan D. Correlation of TIRADS and bethesda scoring systems with final histopathology of thyroid nodules an institutional experience. Indian J Otolaryngol Head Neck Surg. 2022 Dec;74Suppl 3:5753-8. doi: 10.1007/s12070-021-02380-8, PMID 36742706.