
Int J Curr Pharm Res, Vol 17, Issue 6, 25-29Original Article
COMPARATIVE ASSESSMENT OF ULTRASOUND-GUIDED BILATERAL ERECTOR SPINAE PLANE BLOCK AND LOCAL ANAESTHETIC INFILTRATION FOR PERIOPERATIVE PAIN MANAGEMENT IN LUMBAR SPINE FUSION SURGERIES
KANDIKONDA KOTESHWAR1*, KOTHAPALLI TEJA SRI RAKESH2, NANNA VARUN KOUSHIK3
1Department of Anaesthesiology, Government Medical College and General Hospital, Mahabubabad, Telangana, India. 2Department of Anaesthesiology, Government Medical College and General Hospital, Sangareddy, Telangana, India. 3Department of Emergency Medicine, Government Medical College and General Hospital, Mahabubabad, Telangana, India
*Corresponding author: Kandikonda Koteshwar; *Email: koteshwar365@gmail.com
Received: 12 Aug 2025, Revised and Accepted: 02 Oct 2025
ABSTRACT
Objective: Effective management of postoperative pain is essential in lumbar spine fusion surgeries to promote early mobility and minimize side effects associated with opioids. This research evaluates the effectiveness of ultrasound-guided bilateral erector spinae plane block (ESPB) in comparison to local anesthetic wound infiltration for managing perioperative pain.
Methods: A randomized, double-blinded, prospective study was carried out on 100 patients (ASA I and II) between the ages of 18 and 60, who were scheduled for elective lumbar spine fusion. Patients were divided into two groups: Group E was given bilateral ESPB consisting of 25 ml of 0.125% levobupivacaine and 4 mg dexamethasone on both sides; Group l received local infiltration with 25 ml of 0.125% levobupivacaine. Pain scores (NRS), duration until first rescue analgesia, total opioid usage within 24 h, Bruggemann Comfort Scale (BCS), and hemodynamic measures were documented.
Results: Group E exhibited notably lower NRS scores at every time point (e. g., 2 h: 1.89±0.79 compared to 4.78±1.17; p<0.0001), extended duration until first rescue analgesia (8.15±2.85 h compared to 1.76±0.69 h; p<0.0001), and decreased tramadol usage (122.50±34.90 mg compared to 276.80±32.45 mg; p<0.0001). Group E demonstrated substantially improved BCS scores and hemodynamic stability.
Conclusion: Bilateral ESPB is a reliable and efficient substitute for local infiltration, offering improved pain management and enhanced patient satisfaction following lumbar spine fusion.
Keywords: Erector Spinae Plane Block, Lumbar Spine Fusion, Postoperative Analgesia, Wound Infiltration, Opioids, Rescue Analgesia
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i6.7063 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Severe pain is frequently experienced after spinal surgeries, especially in the initial few days. It has been observed that timely mobility, prompt discharge, improved functional outcomes, and a decrease in chronic pain development are all positively associated with appropriate pain management during this period [1]. Lumbar spine fusion surgeries often result in moderate to severe pain after the operation because of significant manipulation of soft tissues and bones, which, if not properly addressed, can postpone movement, raise complications, extend hospital stays, and elevate the likelihood of chronic postsurgical pain conditions [2].
Opioids serve as the main treatment for individuals undergoing spinal surgery. Opioid-based analgesia is associated with various side effects like sedation, respiratory depression, postoperative nausea and vomiting (PONV), itching, urinary retention, and the potential for opioid dependence [3]. These constraints have prompted a change in approach to multimodal analgesia methods, integrating regional anesthesia practices that reduce opioid consumption while enhancing pain management.
The erector spinae plane block (ESPB), introduced by Forero et al. in 2016 [4], is an evolving regional method for thoracic and lumbar surgical procedures. This procedure consists of administering a local anesthetic into the fascial plane located deep to the erector spinae muscle, producing pain relief over several dermatomes. The ESP block is becoming more popular because of its ease of management, safety characteristics, and capability to deliver both somatic and visceral pain relief [5].
In contrast, local anesthetic wound infiltration is a simpler and commonly utilized technique for perioperative pain relief in spine surgery. It entails the insertion of local anesthetic into the subcutaneous and muscle layers of the surgical site at the conclusion of the operation [6].
This study aims to evaluate the pain-relieving effectiveness of ultrasound-guided bilateral ESP block in comparison to local anesthetic wound infiltration in individuals undergoing lumbar spine fusion surgery. This study directly assesses pain severity through the Numerical Rating Scale (NRS), the duration until the initial rescue analgesic, overall opioid usage within the first 24 h, and patient satisfaction ratings using the Bruggemann Comfort Scale.
MATERIALS AND METHODS
Study design
This prospective, randomized, double-blinded study was conducted for a period of 1 y at a Rural Hospital in South India. Institutional Ethics Committee approval and informed patient consent were obtained prior to enrolment.
Participants
A total of 100 patients (ASA I and II), aged 18 to 60 y, scheduled for elective lumbar spine fusion surgery were randomly assigned into two groups of 50 using the closed envelope method.
Inclusion criteria
Age 18 to 60 y
ASA physical status I and II listed for Elective lumbar spine fusion surgery
Exclusion criteria
ASA III or IV
Allergy to local anesthetics
Local infection at the injection site
Preoperative opioid dependence
Coagulopathy or use of anticoagulants
Patient refusal
Group allocation
Group E (ESPB): Administered bilateral ultrasound-guided ESPB using 25 ml of 0.125% levobupivacaine and 4 mg dexamethasone on each side.
Group l (Wound Infiltration): Administered 25 ml of 0.125% levobupivacaine injected at the surgical incision location.
Blinding
Blocks were given by anesthesiologist, and postoperative evaluation was conducted by a different anesthesiologist who was unaware of the group assignment.
Methodology
All patients received comprehensive preoperative evaluations and were apprised of the study and potential complications, after which written consent was secured. On the surgery day, patients were transferred to the operating room, intravenous access was established, and standard ASA monitoring began. Premedication consisted of glycopyrrolate, midazolam, and fentanyl; induction utilized propofol and vecuronium, with maintenance through sevoflurane and a vecuronium infusion. After General Anaesthesia, patients were placed in a prone position.
Assessment parameters
Pain severity measured with the Numerical Rating Scale (NRS) at 0, 2, 4, 6, 12, and 24 h after surgery.
Time to first rescue analgesia-Time when the patient reports pain, a Numerical Rating Scale score of 3 or greater and the duration until the first rescue pain relief are noted.
Total opioid (tramadol) consumption in the first 24 h.
Bruggemann Comfort Scale (BCS) scores.
Hemodynamic parameters (HR, SBP, DBP, SpO₂).
Statistical analysis
Data were analyzed using IBM SPSS v21. Continuous variables were analyzed using the independent t-test, and categorical variables using the chi-square test. A p-value<0.05 was considered statistically significant.
Observations and results
Table 1 indicates that there is no notable difference in demographics among the groups. Average age was 45.10±11.92 y (Group E) compared to 44.70±11.68 y (Group L), p = 0.874; gender distribution was the same (p<0.05).
Table 1: Demographic profile
| Variable | Group E (ESPB) | Group l (Wound infiltration) | p-value |
| mean Age (years) | 45.10±11.92 | 44.70±11.68 | 0.874 |
| Gender (Male/Female) | 29/21 | 28/22 | 1.000 |
Table 2 shows that baseline hemodynamic parameters (HR, SBP, DBP) were comparable between the two groups (p>0.05) at baseline, indicating no initial difference. However, from 30 min to 24 h postoperatively, Group E consistently demonstrated significantly lower heart rate and blood pressure values (p<0.05), reflecting better analgesia and hemodynamic stability compared to Group L.
Table 2: Hemodynamic parameters (Heart rate, SBP, DBP) at 24 h postoperatively
| Time point | Group | HR (bpm) | SBP (mmHg) | DBP (mmHg) | p-value (HR/SBP/DBP) |
| Baseline | E | 83.45±6.70 | 128.60±7.55 | 81.10±6.45 | 0.468/0.412/0.367 |
| L | 84.20±6.35 | 129.80±8.20 | 82.40±5.98 | ||
| 30 min | E | 80.12±6.21 | 122.45±7.80 | 76.10±5.98 | <0.0001 |
| L | 87.55±5.40 | 131.65±6.98 | 84.50±4.87 | ||
| 60 min | E | 79.40±6.02 | 121.80±6.99 | 75.60±5.90 | <0.0001 |
| L | 88.10±4.95 | 130.85±6.44 | 83.80±4.55 | ||
| 2 h | E | 78.40±6.15 | 120.35±6.55 | 74.45±5.75 | <0.0001 |
| L | 87.45±4.55 | 129.60±5.62 | 82.80±4.12 | ||
| 6 h | E | 77.95±5.50 | 119.50±6.00 | 74.00±5.58 | <0.0001 |
| L | 86.90±4.25 | 128.60±5.05 | 82.10±3.85 | ||
| 24 h | E | 77.15±5.30 | 118.70±5.65 | 73.55±5.40 | <0.0001 |
| L | 86.10±3.95 | 127.80±4.75 | 81.65±3.60 |
Table 3 and fig. 1 show notably reduced NRS pain scores in Group E at every measured time point—for instance, at 2 h: 1.89±0.79 compared to 4.78±1.17 (p<0.05), indicating enhanced analgesia from ESPB.
Table 3: Numerical rating scale (NRS) scores
| Time interval | Group E (Mean±SD) | Group l (Mean±SD) | p-value |
| 0 hour | 1.76±0.58 | 5.10±1.09 | <0.0001 |
| 2 h | 1.89±0.79 | 4.78±1.17 | <0.0001 |
| 4 h | 2.11±0.72 | 4.24±0.89 | <0.0001 |
| 6 h | 2.47±0.56 | 4.39±0.90 | <0.0001 |
| 12 h | 1.98±0.45 | 3.55±0.79 | <0.0001 |
| 24 h | 2.69±0.51 | 3.34±0.81 | <0.0001 |
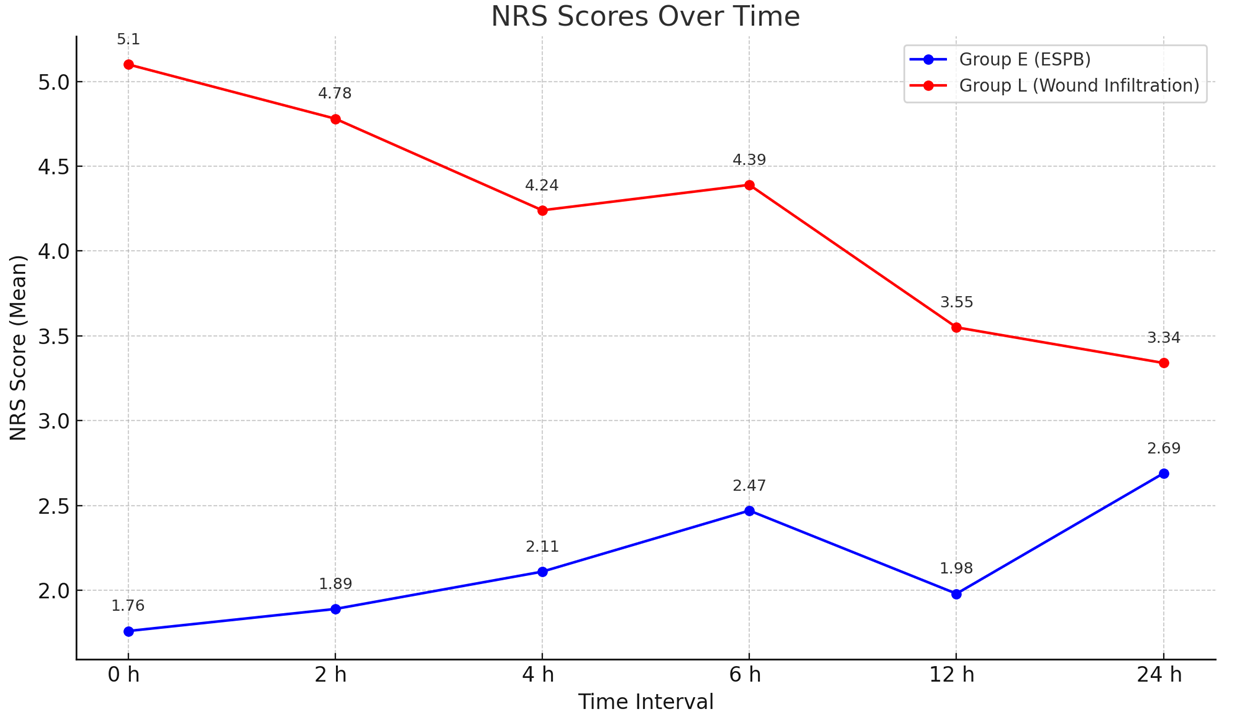
Fig. 1: Line graph showing NRS pain score over time, table 4 indicates that the duration until the first rescue analgesia was markedly greater in Group E (8.15±2.85 h) compared to Group l (1.76±0.69 h), with p<0.05
Table 4: Time to first rescue analgesia
| Group | Mean time (hours) | Standard deviation | p-value |
| Group E (ESPB) | 8.15 | ± 2.85 | <0.0001 |
| Group l (Infiltration) | 1.76 | ± 0.69 | <0.0001 |
Table 5 shows that total tramadol usage in a 24 h period was markedly reduced in Group E (122.50±34.90 mg) relative to Group l (276.80±32.45 mg), p<0.05.
Table 5: Total opioid (Tramadol) consumption
| Group | Mean tramadol consumption (mg) | Standard deviation | p-value |
| Group E (ESPB) | 122.50 | ± 34.90 | <0.0001 |
| Group l (Infiltration) | 276.80 | ± 32.45 | <0.0001 |
Table 6 and fig. 2 show that Group E had greater BCS comfort scores at 2 h (3.32±1.01) compared to Group l (0.94±0.63), with consistent significant differences observed at all time points (p<0.05).
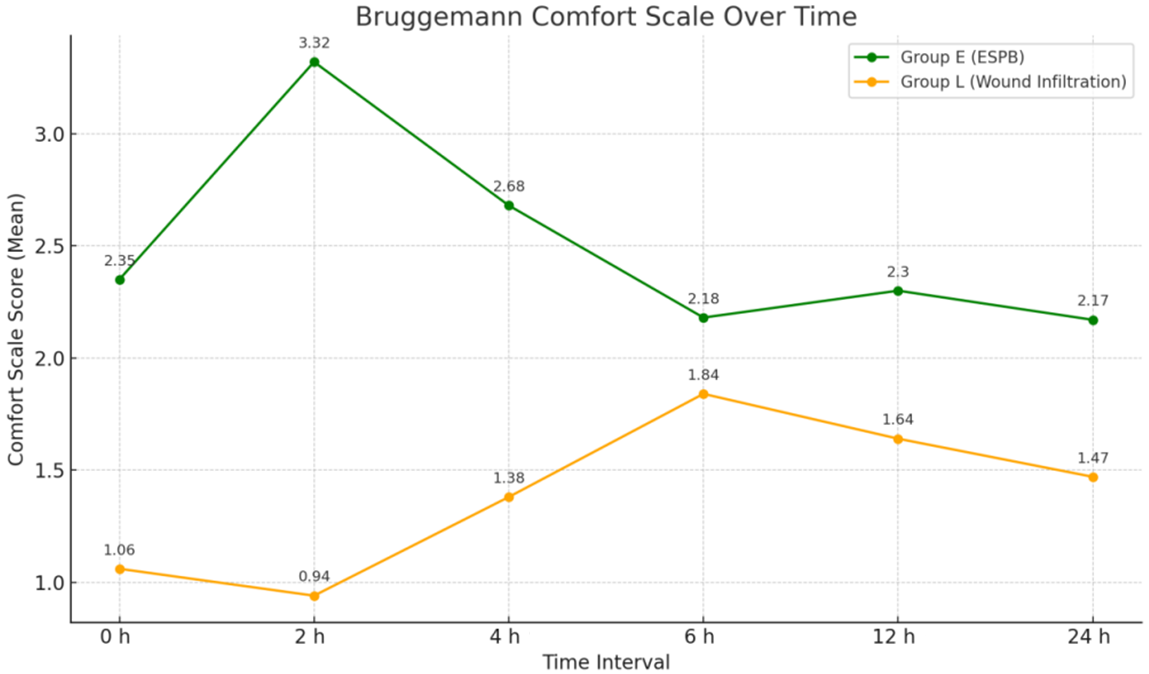
Fig. 2: Line graph showing bruggemann comfort scale between two groups
Table 6: Bruggemann comfort scale (BCS) scores
| Time interval | Group E (Mean±SD) | Group l (Mean±SD) | p-value |
| 0 hour | 2.35±0.98 | 1.06±0.55 | <0.0001 |
| 2 h | 3.32±1.01 | 0.94±0.63 | <0.0001 |
| 4 h | 2.68±0.65 | 1.38±0.54 | <0.0001 |
| 6 h | 2.18±0.59 | 1.84±0.41 | <0.0001 |
| 12 h | 2.30±0.57 | 1.64±0.46 | <0.0001 |
| 24 h | 2.17±0.59 | 1.47±0.52 | <0.0001 |
DISCUSSION
The demographic features of the patients were statistically similar across both groups, removing any baseline bias. The average age in Group E was 45.10±11.92 y, while in Group l it was 44.70±11.68 y, with a p-value of 0.874. The ratio of males to females was also similar (29/21 versus 28/22), with a p-value of 1.000, indicating no notable difference in gender distribution. Similar to our study, Patel et al. in 2025 [7] compared a efficacy of ESPB with Caudal Epidural block for postoperative analgesia after a single-level lumbar fusion surgery. Their results showed no significant differences in age (p = 0.472) and gender (p = 0.862), mirroring our findings where age (p = 0.874) and gender distribution (p = 1.000) likewise revealed no significant differences across groups.
Baseline hemodynamic measures (heart rate, systolic and diastolic blood pressure) were comparable across the groups, with p-values of 0.468, 0.412, and 0.367, indicating no significance at baseline. At every postoperative time point from 30 min to 24 h, Group E consistently demonstrated significantly lower HR, SBP, and DBP values than Group l with statistical significance of (p<0.05), indicating improved hemodynamic stability and diminished stress response attributable to more efficient analgesia. Goyal et al. in 2021 [8] assessed the perioperative impacts of ultrasound-guided ESPB during cervical and thoracic spine procedures and noted a gradual intraoperative reduction in heart rate and mean arterial pressure, suggesting stable hemodynamics during surgery. This trend aligns with our results, as postoperative heart rate, SBP, and DBP were notably reduced in the ESPB group from 30 min to 24 h with the statistical significance of p-value less thsn 0.05.
Pain intensity, assessed through the Numerical Rating Scale, was markedly reduced in Group E across all time points. At the 2-hour mark, Group E had a mean NRS score of 1.89±0.79, compared to 4.78±1.17 for Group l (p<0.05). Similar statistically significant differences were noted at 4, 6, 12, and 24 h (all p<0.05), demonstrating the lasting analgesic efficacy of the ESP block. Asar et al. in 2022 [9], indicated decreased NRS scores at 6, 12, and 24 h (p<0.05), which aligns with our results where Group E exhibited significantly lower NRS scores than Group l across all time points (2 h: 1.89±0.79 vs 4.78±1.17). In both the studies, the ESPB group exhibited notably lower NRS scores.
In Group E, the time to first rescue analgesia was notably extended, averaging 8.15±2.85 h, while in Group l it was only 1.76±0.69 h (p<0.05). This indicates that the ESP block offered more enduring pain relief, postponing the requirement for additional analgesics. In line with this, the overall opioid intake within 24 h was markedly reduced in Group E (122.50±34.90 mg) compared to Group l (276.80±32.45 mg), showing a p-value<0.05. Sangireddy Kavya Sree et al. in 2024 [10] investigated the effectiveness of ESPB versus caudal block in lumbar spine procedures and found that the average length of analgesia in the ESPB cohort was 7:28±1.00 h, whereas it was 4:04±1.00 h for the caudal cohort. In our study, the time to first rescue analgesia was extended in the ESPB group compared to the local infiltration group, suggesting that ESPB reliably offers extended postoperative analgesia in various comparative contexts.
The ESPB group also showed a significantly higher level of patient comfort, evaluated through the Bruggemann Comfort Scale (BCS). At the 2-hour mark, Group E indicated a mean BCS of 3.32±1.01 compared to 0.94±0.63 in Group l (p<0.05). This pattern persisted across all assessed time points, suggesting that individuals in Group E attained greater comfort levels during the postoperative phase. Wang et al. [11] in 2021, evaluated postoperative comfort utilizing the Bruggemann Comfort Scale and found that ESPB consistently yielded higher BCS scores than TLIP and control groups from 6 to 48 h after surgery. This supports our results, as Group E (ESPB) indicated notably greater BCS scores at each time point with statistical significance of p-value of less than 0.05.
CONCLUSION
This study shows that ultrasound-guided bilateral erector spinae plane block (ESPB) offers better perioperative pain relief than local anesthetic wound infiltration in patients having lumbar spine fusion surgery. Patients in the ESPB group showed notably reduced pain scores, postponed requirement for rescue analgesia, decreased opioid usage, better hemodynamic stability, and elevated comfort levels according to the Bruggemann Comfort Scale. These results highlight the efficacy of ESPB as a safe and effective regional anesthesia method that promotes patient recovery and minimizes dependence on systemic opioids, advocating for its wider use in multimodal analgesia strategies for spinal surgeries.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICT OF INTERESTS
Declared none
REFERENCES
Bajwa SJ, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. J Craniovertebr Junction Spine. 2015 Jul-Sep;6(3):105-10. doi: 10.4103/0974-8237.161589, PMID 26288544.
Bheemanna NK, Nagaraj A, Appajigowda NM. Ultrasound-guided bilateral erector spinae block with dexamethasone for post-operative analgesia in lumbar spine surgery: a case series. AACC. 2023;9(3):211-4. doi: 10.18502/aacc.v9i3.13115.
Bohringer C, Astorga C, Liu H. The benefits of opioid free anesthesia and the precautions necessary when employing it. Transl Perioper Pain Med. 2020;7(1):152-7. PMID 31712783.
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016 Sep-Oct;41(5):621-7. doi: 10.1097/AAP.0000000000000451, PMID 27501016.
Siddiqui N, Krishnan S, Dua A, Cascella M. Erector spinae plane block. In: Treasure Island, FL: StatPearls Publishing; Updated 2025 May 3. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545305.
Stamenkovic DM, Bezmarevic M, Bojic S, Unic Stojanovic D, Stojkovic D, Slavkovic DZ. Updates on wound infiltration use for postoperative pain management: a narrative review. J Clin Med. 2021 Oct 11;10(20):4659. doi: 10.3390/jcm10204659, PMID 34682777.
Patel Y, Ramachandran K, Shetty AP, Chelliah S, Subramanian B, Kanna RM. Comparison between relative efficacy of erector spinae plane block and caudal epidural block for postoperative analgesia in lumbar fusion surgery a prospective randomized controlled study. Glob Spine J. 2025 Mar;15(2):639-47. doi: 10.1177/21925682231203653, PMID 37737097.
Goyal A, Kalgudi P, Sriganesh K. Ultrasound-guided erector spinae plane block for perioperative analgesia in cervical and thoracic spine surgeries a case series. Neurol India. 2021;69(2):487-9. doi: 10.4103/0028-3886.314568, PMID 33904483.
Asar S, Sarı S, Altinpulluk EY, Turgut M. Efficacy of erector spinae plane block on postoperative pain in patients undergoing lumbar spine surgery. Eur Spine J. 2022 Jan;31(1):197-204. doi: 10.1007/s00586-021-07056-z, PMID 34802140.
Sree SK, Prakash BC, Gangadhar SB. Comparative evaluation of ultrasound-guided bilateral erector spinae block and ultrasound guided caudal block in lumbar spine surgeries for post-operative analgesia. Int J Pharm Clin Res. 2024;16(9):843-9.
Wang L, Wu Y, Dou L, Chen K, Liu Y, Li Y. Comparison of two ultrasound-guided plane blocks for pain and postoperative opioid requirement in lumbar spine fusion surgery: a prospective randomized and controlled clinical trial. Pain Ther. 2021 Dec;10(2):1331-41. doi: 10.1007/s40122-021-00295-4, PMID 34346027.