
Int J Curr Pharm Res, Vol 17, Issue 6, 48-51Original Article
EFFICACY OF ULTRASOUND-GUIDED SAPHENOUS NERVE BLOCK USING BUPIVACAINE ALONE VERSUS BUPIVACAINE WITH TRIAMCINOLONE ACETONIDE IN OSTEOARTHRITIS KNEE PAIN
ARJUN PIRKAD1*, SUHEELA TAXAK2, DRPOONAM SINGH3
1MGM Medical College and Hospital, Kamothe, Maharashtra, India. 2,3Institute of Medical Science, Rohtak, Haryana, India
*Corresponding author: Arjun Pirkad; *Email: arjunpirkad@gmail.com
Received: 12 Aug 2025, Revised and Accepted: 02 Oct 2025
ABSTRACT
Objective: Knee osteoarthritis (OA) is a prevalent cause of chronic pain and functional impairment. Ultrasound-guided saphenous nerve block has emerged as a promising non-surgical treatment modality. This study evaluates the comparative efficacy of bupivacaine alone versus bupivacaine with triamcinolone acetonide in ultrasound-guided saphenous nerve block for OA knee pain.
Methods: A prospective, randomized, double-blind study was conducted involving 80 patients aged 30–80 y with chronic OA knee pain (Grade II or III). Patients were allocated to two groups: Group T received 4 ml of 0.5% bupivacaine+40 mg triamcinolone acetonide; Group B received 4 ml of 0.5% bupivacaine alone. Both solutions were diluted to 10 ml with normal saline. Pain intensity (VAS), functional disability (WOMAC index), and patient satisfaction were assessed at baseline, 1 h, 1 w, 2 w, 1 mo, 3 mo, and 6 mo post-block.
Results: Both groups showed significant reductions in VAS and WOMAC scores over time (p<0.05). However, Group T showed superior pain relief and functional improvement at all follow-up points (p<0.05). Grade II OA patients in both groups had better outcomes compared to Grade III. No significant procedural complications were noted.
Conclusion: Ultrasound-guided saphenous nerve block using bupivacaine with triamcinolone acetonide provides prolonged and superior analgesia and functional improvement compared to bupivacaine alone in patients with OA knee. This technique is safe, effective, and minimally invasive, warranting consideration in non-surgical OA knee management.
Keywords: Knee osteoarthritis, Saphenous nerve block, Ultrasound-guided block, Bupivacaine, triamcinolone acetonide, Chronic knee pain
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i6.7074 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Osteoarthritis (OA) of the knee is a chronic, progressive degenerative joint disorder that severely impairs quality of life, especially in the elderly [1, 2]. It is characterized by loss of articular cartilage, bone remodeling, pain, stiffness, and reduced joint mobility [3, 4]. The global burden of knee OA continues to rise due to aging populations and increasing obesity rates [5, 6]. Despite various treatment options, effective long-term relief from chronic knee pain remains a clinical challenge [7].
Conventional pharmacological therapies such as NSAIDs and opioids are often limited by side effects and contraindications [8, 9]. Intra-articular injections provide only short-term relief, and surgical options may not be suitable for all patients due to age, comorbidities, or personal preference [10, 11]. Therefore, minimally invasive regional nerve blocks under ultrasound guidance offer a promising alternative to bridge this gap [12, 13].
The saphenous nerve, a purely sensory branch of the femoral nerve, supplies the anteromedial aspect of the knee [14]. It travels through the adductor canal and becomes superficial in the distal thigh, making it an ideal target for ultrasound-guided blockade [15, 16]. Bupivacaine, a long-acting amide local anesthetic, is widely used in peripheral nerve blocks due to its potent analgesic properties [17, 18]. The addition of corticosteroids like triamcinolone acetonide is hypothesized to prolong analgesic effects by reducing inflammation and suppressing ectopic neuronal discharge [19-21].
This study aims to evaluate the efficacy of ultrasound-guided saphenous nerve block using bupivacaine alone versus bupivacaine with triamcinolone acetonide in patients with chronic knee pain due to OA.
MATERIALS AND METHODS
This prospective, randomized, double-blind study was conducted at the Department of Anaesthesia and Intensive Care, Pt. B. D. Sharma PGIMS, Rohtak.
Inclusion criteria
Grade II/III OA knee pain
Age 30–80
VAS>40 mm
Non-responsive to 4 w of conservative therapy
Exclusion criteria
Drug allergy
Neuropathy
Coagulopathy/infection
Severe hepatic/renal dysfunction
Pregnancy/previous knee surgery
Groups
A total of 80 patients were randomly and equally divided into two groups. Group T and Group B.
Group T (n=40): 4 ml 0.5% bupivacaine+40 mg triamcinolone acetonide (diluted to 10 ml)
Group B (n=40): 4 ml 0.5% bupivacaine diluted to 10 ml
Procedure
The saphenous nerve was blocked under ultrasound guidance 10 cm above the knee joint line using a 23-G needle and linear probe. Local infiltration with 2% lignocaine was done before injection.
Post-procedure care
Paracetamol 500 mg three times daily for 3 days. Rescue analgesia with diclofenac 50 mg TID if VAS>40 mm.
Outcomes parameters
Pain score
Pain was measured using the Visual Analog Scale (VAS; 0–100 mm) during activities such as sitting, standing, walking, and bending. Assessments were done 30 min before the block, and at 1 h, 1 w, 2 w, 1 mo, 3 mo, and 6 mo post-procedure [22].
Quality of life
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) is a three-dimensional, self-administered questionnaire that evaluates pain (5 items), stiffness (2 items), and physical function (17 items). Scores were calculated by averaging the total and converting it to a percentage disability. The WOMAC index was calculated before giving block, 1 h, 1 w, 2 w, 1 mo, 3 mo, and 6 mo after giving block on a four-point scale [23].
Patient satisfaction
Rated on a four-point scale (Excellent to Poor) based on pain reduction:
Excellent: ≥75% reduction
Good: 50–74%
Fair: 25–49%
Poor: <25% or increased pain assessed at 1 h, 1 w, 2 w, 1 mo, 3 mo, and 6 mo post-block.
Statistical analysis
Data were analyzed using SPSS version 18.0. Unpaired t-test was used to compare means between groups, paired t-test for within-group comparisons over time, and Chi-square test for nominal data. A p-value< 0.05 was considered statistically significant at a 95% confidence level.
RESULTS
A total of 80 patients aged between 30-80 y with VAS>40 mm and osteoarthritis grade II and III. Were included in the study. The patients were randomly allocated to one of the two groups, comprising 40 patients in each group.
In terms of demographic data. Group T had a mean age of 56.70±9.99 y and weight of 62.22±7.90 kg; Group B had 54.58±8.72 y and 64.60±7.83 kg, respectively. Male: Female ratio was 13:27 in Group T and 11:29 in Group B. Differences were not statistically significant (p > 0.05) in both groups as displayed in fig. 1.
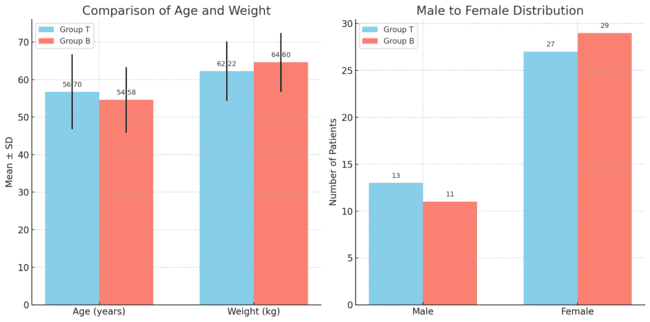
Fig. 1: Demographic distribution, the Kellgren and Lawrence grades based on X-ray findings of knee osteoarthritis were comparable between groups, with no significant difference (p > 0.05). Group T had 50% each of Grade II and III, while Group B had 55% Grade II and 45% Grade III cases as displayed in fig. 2
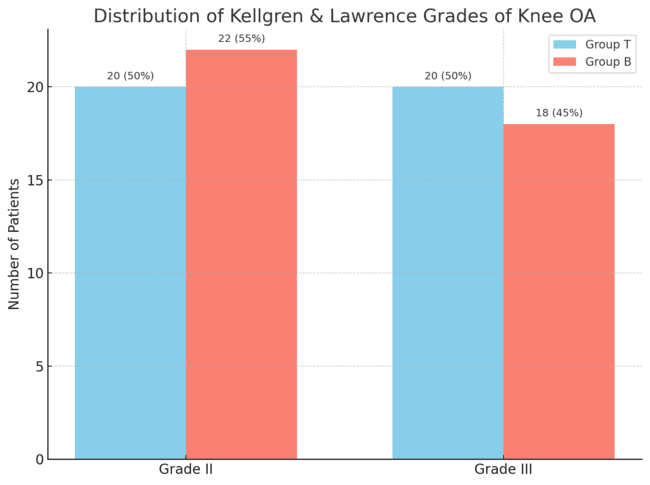
Fig. 2: Kellgren and lawrence grades, visual analogue scale (VAS) pain scores between Group T and Group B over various time points are depicted in table 1
Table 1: VAS score comparison between groups T and B
| Time point | Group T (Mean±SD) | Group B (Mean±SD) | p-value |
| Baseline | 74.13±11.03 | 73.50±10.67 | 0.644 |
| 1 H Post-Block | 1.75±3.85 | 2.10±4.39 | 0.419 |
| 1 W | 5.13±5.94 | 11.13±7.47 | 0.001 |
| 2 W | 11.75±5.13 | 23.50±14.77 | 0.001 |
| 1 Mo | 18.63±11.27 | 34.75±10.00 | 0.001 |
| 3 Mo | 24.63±5.36 | 54.13±6.88 | 0.001 |
| 6 Mo | 32.00±4.35 | 58.13±6.27 | 0.001 |
At baseline, both groups had similar pain scores (p = 0.644). However, from 1 w onward, Group T consistently showed significantly lower VAS scores compared to Group B (p = 0.001 at all time points), indicating greater and sustained pain relief in Group T following the saphenous nerve block. The Western Ontario and McMaster Universities (WOMAC) index of osteoarthritis was compared between both groups at various time intervals, as displayed in table 2.
Table 2: WOMAC index scores between groups T and B
| Time point | Group T (Mean±SD) | Group B (Mean±SD) | p-value |
| Baseline | 78.3±6.2 | 76.9±6.5 | 0.318 |
| 1 H | 10.2±2.4 | 12.5±2.8 | 0.020 |
| 1 W | 18.9±5.3 | 28.7±6.1 | 0.001 |
| 2 W | 23.6±5.8 | 36.2±7.0 | 0.001 |
| 1 Mo | 31.1±6.2 | 48.3±7.5 | 0.001 |
| 3 Mo | 38.4±6.0 | 61.5±8.4 | 0.001 |
| 6 Mo | 43.7±6.5 | 65.0±8.1 | 0.001 |
Both groups had similar baseline scores (p = 0.318), indicating comparable initial disability. However, from 1 h post-block onward, Group T consistently demonstrated significantly lower WOMAC scores than Group B (p < 0.05 at all time points), reflecting better improvement in pain, stiffness, and physical function in Group T over the 6-month follow-up period.
DISCUSSION
Osteoarthritis (OA) is a debilitating condition characterized by pain, joint inflammation and joint stiffness and results in a substantial degree of physical disability. It is most common form of arthritis and exerts significant burden on individual and family. It is a major cause of distress and disability, with reduced quality of life and increased healthcare expenditure [1, 2, 5, 8]. Age, race, genetics, body build, obesity, gender, occupational factors, repetitive use and previous injury have all been shown to have an influence to development of OA knee [5].
Goals of osteoarthritis treatment include alleviation of pain and improvement of functional status. Optimally, patients should receive a combination of nonpharmacologic and pharmacologic treatment. These current therapies that help alleviate joint pain have limited effectiveness by certain drugs and procedures; produce unwanted side effects, thereby precluding their long-term use. There is clearly a need to find out some other alternative methods that are simple, effective, efficacious, minimally invasive, widely acceptable and applicable that gives better results. One such promising method is ultrasound-guided saphenous nerve block [15].
Saphenous nerve block gives complete anterior and medial knee pain relief and as most of the knee OA patients have anterio-medial knee pain. It has been successfully used for postoperative pain relief after total knee replacement. Local anaesthetics in combination with steroid are commonly used for prolonged pain relief in many chronic musculosketal conditions like back pain [19, 20].
In our study we have used ultrasound guided saphenous nerve block in knee OA patients where forty patients received 4 ml of 0.5% bupivacaine with 40 mg (1 ml) of triamcinolone acetonide diluted to normal saline to a total 10 ml solution (Group T) and the remaining forty received 4 ml of 0.5% bupivacaine diluted to normal saline to a total 10 ml solution (Group B) and these patients were followed-up at intervals of one hour, one week, two weeks, one month, three months and six months with respect to providing pain relief, improvement in functional disability, need of repeat block and procedural complications.
Group T showed statistically and clinically superior results in both VAS and WOMAC scores. Previous studies have shown the efficacy of corticosteroids when used with local anesthetics for prolonging analgesia [19-21]. This block targets the sensory fibers of the knee without affecting motor function [21].
No complications such as bleeding, infection, or neuropathy were noted in either group, affirming the safety of the ultrasound-guided technique [15, 16].
CONCLUSION
Ultrasound-guided saphenous nerve block using bupivacaine with triamcinolone acetonide significantly improves pain and function in knee OA compared to bupivacaine alone. It is safe, effective, and should be considered for patients unfit for surgery or unresponsive to conservative therapy [15, 16].
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICT OF INTERESTS
Declared none
REFERENCES
Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41(8):1343-55. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9, PMID 9704632.
WHO Scientific Group. The burden of musculoskeletal conditions at the start of the new millennium. World Health Organ Tech Rep Ser. 2003;919:1-128.
Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;21(9):1145-53. doi: 10.1016/j.joca.2013.03.018, PMID 23973124.
AAOS. Treatment of osteoarthritis of the knee. In: Evidence-based guideline. 2nd ed. Rosemont: Am Acad Orth Surg; 2013. doi: 10.5435/JAAOS-21-09-571.
Hart DJ, Doyle DV, Spector TD. Incidence and risk factors for radiographic knee osteoarthritis in middle-aged women: the Chingford Study. Arthritis Rheum. 1999;42(1):17-24. doi: 10.1002/1529-0131(199901)42:1<17::AID-ANR2>3.0.CO;2-E, PMID 9920009.
Goldring SR, Goldring MB. Clinical aspects pathology and pathophysiology of osteoarthritis. J Musculoskelet Neuronal Interact. 2006;6(4):376-8. PMID 17185832.
Watson M. Management of patients with osteoarthritis. Pharm J. 1997;259:296-7.
Michael JW, Schluter Brust KU, Eysel P. The epidemiology etiology diagnosis and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107(9):152-62. doi: 10.3238/arztebl.2010.0152, PMID 20305774.
Goldring SR, Goldring MB. Clinical aspects pathology and pathophysiology of osteoarthritis. J Musculoskelet Neuronal Interact. 2006;6(4):376-8. PMID 17185832.
Dieppe PA, Sathapatayavongs B, Jones HE, Bacon PA, Ring EF. Intra-articular steroids in osteoarthritis. Rheumatol Rehabil. 1980;19(4):212-7. doi: 10.1093/rheumatology/19.4.212, PMID 7010511.
Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res. 1994;(301):221-6. doi: 10.1097/00003086-199404000-00034, PMID 8156678.
Partownavid P. Ultrasound-guided peripheral nerve block. Am J Ther. 2009;16(4):304-12. doi: 10.1097/MJT.0b013e3181715684, PMID 19531938.
Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34(6):578-80. doi: 10.1097/aap.0b013e3181bfbf84, PMID 19916251.
Eckmann MS. Saphenous nerve block shows promise for chronic knee pain. Int Anesth Res Soc. 2009 Aug 7(8):11.
Harshe R. Prolonged knee pain relief by saphenous block (new technique). Indian J Pain. 2013;27(1):36-40. doi: 10.4103/0970-5333.114871.
Loteroa MA, Diazb RR, Mejia Aguilarc MA, Jaramillo SJ. Efficacy and safety of ultrasound-guided saphenous nerve block in patients with chronic knee pain. Colomb J Anestn. 2014;42(3):166-71. doi: 10.1016/j.rca.2014.03.005.
Tsai PB, Karnwal A, Kakazu C, Tokhner V, Julka IS. Efficacy of an ultrasound-guided subsartorial approach to saphenous nerve block: a case series. Can J Anaesth. 2010;57(7):683-8. doi: 10.1007/s12630-010-9317-1, PMID 20428987.
Lin Y, Liu SS. Local anesthetics. In: Barash PG, Cullen B, Stoelting RK, Chahalan MK, Stock MC, Rafeal O, editors. Clinical Anesthesia. 7th ed. Philadelphia: Lippincott; 2013. p. 562-8.
Mackinnon SE, Hudson AR, Gentili F, Kline DG, Hunter D. Peripheral nerve injection injury with steroid agents. Plast Reconstr Surg. 1982;69(3):482-90. doi: 10.1097/00006534-198203000-00014, PMID 7063571.
Stan T, Goodman EJ, Bravo Fernandez C, Holbrook CR. Adding methylprednisolone to local anesthetic increases the duration of axillary block. Reg Anesth Pain Med. 2004;29(4):380-1. doi: 10.1016/j.rapm.2004.03.006, PMID 15305267.
Devor MD, Govrin Lippmann R, Raber P. Corticosteroids suppress ectopic neural discharge originating in experimental neuromas. Pain. 1985;22(2):127-37. doi: 10.1016/0304-3959(85)90173-3, PMID 4047699.
Hooten WM. Assessment and management of chronic pain. Institute for Clinical Systems Improvement. 2013;6:1-105.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833-40. PMID 3068365.