
Int J Curr Pharm Res, Vol 17, Issue 6, 57-61Original Article
ANALYSIS OF BLOOD DONOR DEFERRAL PATTERN AT BLOOD CENTRES OF TERTIARY CARE HOSPITAL IN CHENNAI, TAMIL NADU-A RETROSPECTIVE CROSS SECTIONAL STUDY
CHITRA M.1, ANBARASI A.2, RAVISHANKAR J.3*
1Department of Transfusion Medicine, Kalaignar Centenary Super Specialty Hospital, Guindy, Chennai, Tamilnadu, India. 2Department of Transfusion Medicine, Government Royapettah Hospital, Chennai, Tamilnadu, India. 3Department of Immunohematology and Blood Transfusion, Government Tirunelveli Medical College Hospital, Tirunelveli, Tamilnadu, India
*Corresponding author: Ravishankar J.; *Email: ravishankar@tvmc.ac.in
Received: 09 Aug 2025, Revised and Accepted: 07 Oct 2025
ABSTRACT
Objective: Even though blood transfusion is a life-saving procedure, selecting a blood donor whose blood is safe for the recipient patient while avoiding adverse donor reaction is paramount in blood transfusion services. During this process, donors can get deferred which leads to loss of precious blood units. This cross-sectional retrospective study was designed to learn and analyze the reasons for deferral of blood donors at tertiary care hospital blood centres.
Methods: This was a retrospective cross-sectional study with analysis of data for one year (April 2024 to March 2025) in May 2025. Blood donor details from Kalaignar Centenary Hospital blood centre and Government Royapettah Hospital blood centre at Chennai, Tamil Nadu were collected from Donor questionnaire forms and deferred donor register. Data was entered in Microsoft excel and analysed.
Results: Among 7877 blood donors who had registered at the blood centres during study period, donor deferral rate was 2.73%(n=215/7877) which was more common in males (78.6%, n=169/215). Most common reason of temporary deferral was low Haemoglobin (28.1%, n=43/153) followed by Hypertension (12.42%, n=19/153). Among the permanent deferrals who were all males (100%, n=62/62), the most common reason was seroreactivity to Hepatitis B virus (62.9%, n=39/62).
Conclusion: Our study findings suggest that more awareness about donation criteria and health education in population are needed, to avoid blood donor deferrals. Effective measures need to be established to bring back the temporarily deferred donors into blood donation donor pool.
Keywords: Blood donors, Donor deferral, Hepatitis B
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i6.7078 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
In current medical and surgical practice, blood transfusion is a life‑saving procedure. The main goal of blood transfusion services (BTS) worldwide is ensuring the availability of safe and adequate supply of blood and blood products [1].
As the world population increases with ease of access to better healthcare, there is a growing demand for blood components [2]. This requires recruiting safe donors and preventing high-risk donors from donating. Selecting a blood donor whose blood is safe for the recipient patient while avoiding adverse donor reaction is paramount in blood transfusion services. Risk of transmission of infective agents can be reduced with strict implementation of donor selection criteria [2, 3].
In countries which are newly establishing blood transfusion services or those countries which are strengthening their already existing services, guidelines for donor selection criteria are laid down by the World Health Organization. In India, the third edition of Transfusion Medicine technical manual released by Government of India in 2023 tabulates the criteria for donor selection and deferral intervals for all blood centres [4, 5].
Generally, blood donors are perceived to be healthy. But some donors may be unsuitable or unfit for blood donation. Such donors should be identified and deferred either temporarily or permanently. However, frequent donor deferral, especially temporary, leads to potential loss of blood donors and many are reluctant to return in future for donation because of negative psychological impact [6]. This shortage due to donor deferrals and loss of blood units from improper collection are more common than shortage due to disease marker testing [3].
Analysis of reasons for deferral of donors helps blood centres in fine-tuning their methods of donor screening, knowing the current health of donors, understanding cultural practices in the general population and measures for retaining donors who were deferred temporarily [7, 8].
The aim of the present study was to learn and analyze the reasons for deferral of blood donors at tertiary care hospital blood centres.
MATERIALS AND METHODS
This retrospective cross-sectional study was conducted at the blood centres of tertiary care referral hospitals at Chennai (Kalaignar Centenary Super Specialty Hospital, Guindy and Government Royapettah Hospital) between April 2024 and March 2025. The study was approved by Institutional ethics committee. All potential blood donors were evaluated based on donor questionnaire, hemoglobin estimation and physical examination. Hemoglobin was measured by specific gravity methods using copper sulphate solution. The criteria given in Transfusion Medicine technical Manual, third edition was used for deciding suitability and deferral of blood donors. Informed consent was obtained before enrolment. The details of blood donors were retrieved from deferred donor registry and blood donor questionnaire form.
Statistical analysis
Data collected was tabulated using Microsoft Excel (Microsoft Corporation, Washington, USA). Data analysis was performed using SPSS statistical software suite version 20 (IBM, USA). Descriptive statistical measures (frequency and percentage), were utilized to present the data.
RESULTS
A total of 7877 donors had registered to voluntarily donate blood at the two blood centres during the study period. 2.73% of these registered donors were deferred from donation (n=215/7877) (table 1). Almost half of the deferred donors were in the age group of 18-30 y (49.76%, n=107/215) followed by donors in the age group of 31-50 y (36.28%, n=78/215) (fig. 1). Most of these donors were males (95.92%, n=7556/7877) (table 1, fig. 2). Most of the deferred donors were males (78.6%, n=169/215). But the deferral rate was less in males (2.24%, n=169/7556) when compared to female donors (14.33%, n=46/321). The ABO blood group of the deferred blood donors were in the order O>B>A>AB (table 2).
Table 1: Frequency of donor deferral
| Gender | Registered donors | Deferred donors |
| Male | 7556(95.92%) | 169/215(78.6%) |
| Female | 321(4.05%) | 46/215(21.4%) |
| Total | 7877 | 215 |
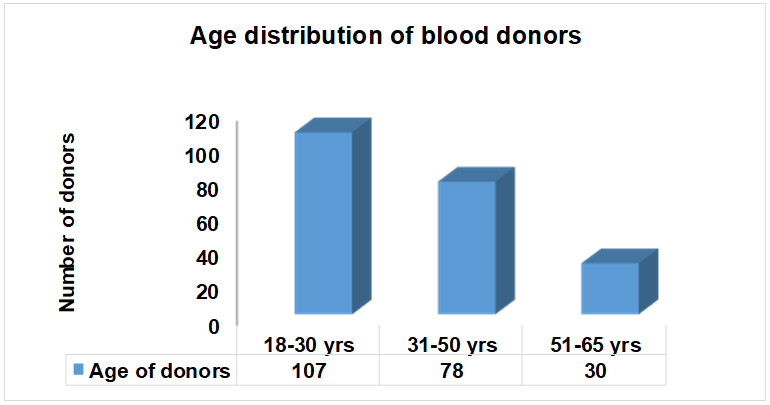
Fig. 1: Age distribution of blood donors in the present study, (n = 7877)
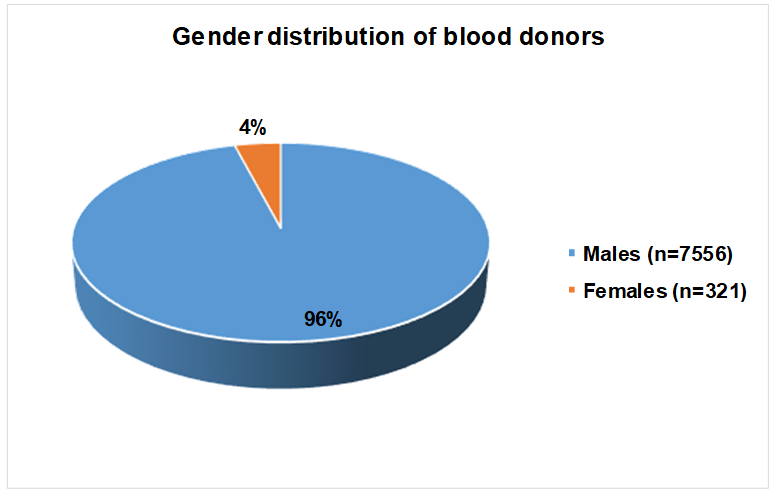
Fig. 2: Gender distribution of blood donors in the present study, (n = 7877)
Table 2: Distribution of blood group among blood donors
| Blood group | Number of donors |
| A positive | 36 |
| B positive | 63 |
| O positive | 93 |
| AB positive | 14 |
| A Negative | 3 |
| B Negative | 2 |
| O Negative | 1 |
| AB Negative | 3 |
Donor deferrals were categorized into two types, temporary and permanent. Temporary deferrals were more common, constituting 71.16% (n=153/215) of all deferrals, compared to 28.83 % (n=62/215) for permanent deferrals. Most of the temporarily deferred donors were males, 69.93% (n=107/153) (table 1). In the permanent deferral category, all were males (100%, n=62/62).
The most common reason for temporary deferrals was low haemoglobin levels, accounting for 28.10% (n=43/153) of all temporary deferrals, followed by donors with hypertension (BP>150/90 mmHg, responsible for 12.42% (n=19/153) (fig. 3).
Hepatitis B virus (HBV) reactivity was the most common cause for permanent donor deferral, accounting for 62.90% (n=39/62) and contributing to 18.14 % of all deferrals. Seizure disorder was the second most frequent cause, representing 11.29% (n=7/62) of permanent deferrals and 3.26 % of total deferrals (fig. 4).
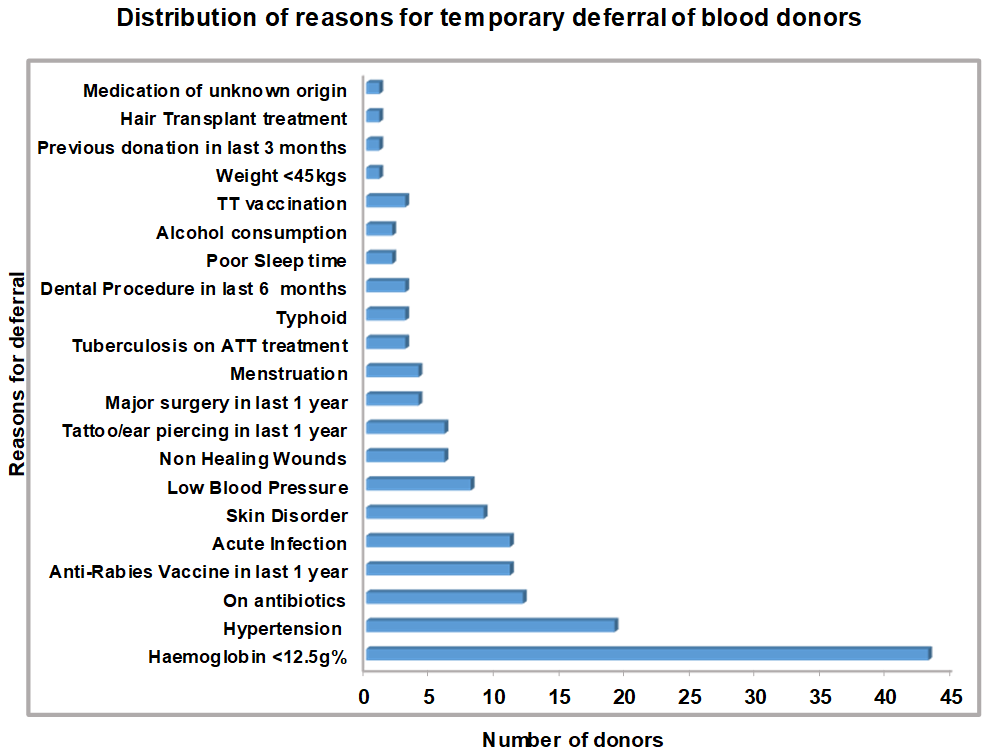
Fig. 3: Reasons for temporary deferral of blood donors, (n=153)
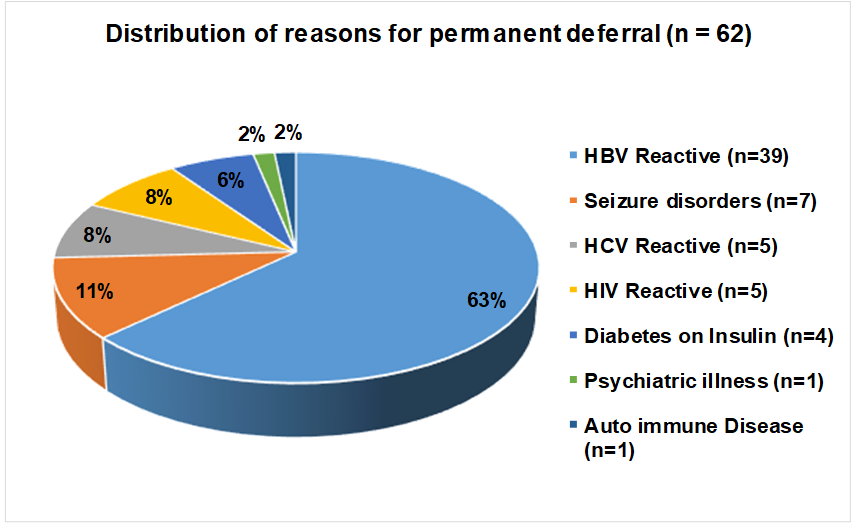
Fig. 4: Reasons for permanent deferral of blood donors (n = 62)
DISCUSSION
Donor selection has vital importance in blood banking and transfusion medicine [5]. Donor deferral is a painful experience for both donors and the blood centres. This also leaves the prospective donors with negative feeling about self as well as blood banking system, when they are deferred.
Blood donation forms an essential part of any community-based health service as the donated blood saves lives of patients. Thus, blood donors form a principal component of this system. But every donor has to undergo and pass the screening procedure before they can donate blood. This is not only for the safety of the intended recipient but also to avoid adverse reactions in the donors, during donation. There are several temporary and permanent reasons for deferral of donors, which can diminish the existing donor pool as well as diminishing the blood components available for the transfusion service. The reasons for deferral of blood donors varies between countries and between regions in the same country. But the challenge is universal in most of the blood centres in all countries [9].
In this study, an attempt has been made to highlight the various reasons for deferral of blood donors, so as to get a better understanding of the deferral pattern in Chennai region.
The rate of deferral differs from region to region and sometimes in same region from one centre to another centre (table 3). The analysis of the donor deferral pattern in specific demographic areas is important to develop a safe pool of blood donors [12].
In our study, most of the donors were males (95.92%). This finding was similar to the study by Unnikrishnan et al. who reported predominantly male donors (95.13%) [17]. John F et al. reported 95.08% males and 4.92% females [18]. As noticed in the present study, the female donor population 4.07% (n=321/7877) was very low. This may be due to lack of awareness, fear, misconception about physiological reasons or lack of motivation.
Table 3: Comparison of data from the present study with other studies in India
| Study | Country | Study period | Total donors | Deferral donor rate (in %) |
Commonest cause of temporary deferral | Commonest cause of permanent deferral |
| Present study | Chennai, India | 1 y | 7877 | 2.73 | Low Hb(Anaemia), Hypertension |
Seropositive for HBV |
| Soundarya V et al. [10] | Chennai, India 2024 | 3 y | 17082 | 5.8 | Low Hb, Alcohol intake within 24 h | Uncontrolled Hypertension |
| Saeed N et al. [11] | Lahore, Pakistan 2024 | 2 y | 6616 | 4.2 | Low Hb | HCV |
| Kujur P et al. [12] | Chattisgarh, India 2020 | 2 y | 18025 | 3.77 | Recent Alcohol intake | Hypertension |
| Ahmad N et al. [9] | New Delhi India 2020 | 7 y | 7806 | 12.6 | Anaemia Hypertension | Hypothyroidism |
| Saravanan S et al. [3] | Tirunelveli India 2023 | 3 y | 29847 | 13.81 | Low Haemoglobin, Medication |
Hypothyroidism |
| Jain V et al. [13] | Baroda India 2021 | 1 y and 4 mo | 13042 | 7.71 | Low Haemoglobin | Hypertension |
| Singh J S et al. [14] | Uttar Pradesh India 2023 | 3 y | 32381 | 6.3 | High Blood pressure | Heart Disease |
| Gurika et al. [5] | Ludhiana India 2024 | 1 y | 22652 | 2.3 | Anaemia | High Blood pressure |
| Rajan R M et al. [15] | Karakonam India 2022 | 4 y and 9 mo | 8064 | 19.1 | Hypertension | Seropositive for HBV |
| Thivya Ret al. [16] | Tamil Nadu India 2021 | 3 y | 7010 | 5.19 | Anaemia | Seropositive for HBV |
In our study, total donor deferral rate was 2.73% which is similar to studies done by Gurika et al. (2.3%), Saeed N et al. (4.2%) and Kujur P et al. (3.77%) [5, 11, 12]. Male donors experienced a high deferral rate of 78.6%. These findings were similar to the results by Saravanan et al. (Males – 84.2%, Females – 15.8%), Ahmad et al. (Males – 81.6%, Females – 18.31%), Soundarya V et al. (Males – 75.8%, Females – 24.2%) and Jain et al. (Males – 88.53%, Females – 12.52%) [3, 9, 10, 13]. Despite their lower deferral rate, males accounted for 78.60 % (n=169/215) of the total deferrals due to their larger representation among donors (n=169/7556), whereas females, though a smaller portion of the donor pool (n=46/321), represented 21.39 % (n=46/215) of the total deferrals. This lower participation but high deferral rates in female donors may be due to reluctancy, fear of needle pain, misbeliefs and high incidence of anemia in females.
In the present study, deferral rate was highest among the 18–30 y age group (49.8%, n=109/215). This was comparable to the studies by Soundarya V et al. (59.9%) and Ahmad N et al. (44.3%) [9, 10]. Out of the 215 donors who were deferred, 71.16% (n=153/215) were deferred temporarily. Deferral of more donors due to temporary reasons compared to permanent reasons was similar to the studies by Gurika et al. (82.8%, n=429/518), Jain et al. (67.30%, n=677/1006) and Singh J S et al. (98.8%, n=2016/2039) [5, 13, 14].
The most common reason for temporary deferral in the present study was low hemoglobin (28.1%, n=43/153) followed by hypertension (12.42%, n=19/153). This was similar to the results seen in the studies by Saravanan S et al. (13.7%), Gurika et al. (32.6%), Jain V et al. (25.7%) and Thivya R et al. (27.75%) but it was higher in the study by Soundarya V et al. (73.7%) [3, 5, 13, 16, 10]. Low hemoglobin can be corrected by increasing the intake of iron rich food and taking iron supplements. These donors can be followed, for blood donation at a later date. Hypertension can due to systemic hypertension per se or due to anxiety, fear of phlebotomy in first time donors and white coat hypertension. They can be made comfortable and relaxed by keeping them in conversation and allaying their fears of donation. Donors who are temporarily deferred can be turned into regular voluntary donors, if the counselor is in constant communication and giving encouragement.
In the present study among permanent reasons for deferral, most common cause was seropositive to HBV infection (62.9 %, n=39/62), which is similar to studies done by Rajan R M et al. (38.24%) and Thivya R et al. (52.3%) [15, 16]. TTI positive blood donors need to counselled and encouraged to get treatment at the respective clinical departments. They should be educated on the risk of transmission and avoidance of further blood donations.
CONCLUSION
Donor deferral was comparatively lower in the present study. Low hemoglobin in donors can be addressed by change in dietary habits and iron supplementation. Continuous awareness and education of donors regarding reasons and duration for temporary deferrals helps in reducing temporary deferral of donors. Constant communication and encouragement can help to retain the donor pool. Donors who are permanently deferred should be counselled for treatment at the appropriate specialty departments. They should be educated on the risk of transmission and avoidance of further blood donations. Documentation and entries in blood bank management systems like Hospital Management Information System (HMIS) and eRaktkosh can help to prevent these donors from donating at other blood centres.
ABBREVIATIONS
BTS – Blood transfusion services
HBV – Hepatitis B virus
HCV – Hepatitis C virus
HMIS – Hospital Management Information System
ACKNOWLEDGMENT
The authors would like to acknowledge all staff at the blood centre for their cooperation and support in conducting this study.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
MC conceptualized the study, collected data and prepared manuscript. JR edited manuscript and analyzed data. AA analyzed data and accepted manuscript.
CONFLICT OF INTERESTS
Declared none
REFERENCES
Ekwere TA, Ino Ekanem M, Motilewa OO, Ibanga IA. Pattern of blood donor deferral in a Tertiary Hospital, South-South, Nigeria: a three-year study review. Int J Blood Transfus Immunohematol. 2014;4:7-13. doi: 10.5348/ijbti‑2014‑14‑OA‑2.
Gillet P, Neijens E. An original approach to evaluating the quality of blood donor selection: checking donor questionnaires and analyzing donor deferral rate. Front Med (Lausanne). 2018 Mar 21;5:74. doi: 10.3389/fmed.2018.00074, PMID 29619370.
Saravanan S, Manimala SA, Parimalam M, Ravishankar J. Analysis of causes for pre-donation deferral among voluntary blood donors at a Tertiary Care Hospital. Asian J Pharm Clin Res. 2023;16(12):128-31. doi: 10.22159/ajpcr.2023.v16i12.48457.
World Health Organization. Blood donor selection: guidelines on assessing donor suitability for blood donation. Geneva: WHO; 2012. Available from: https://www.ncbi.nlm.nih.gov/ books/NBK138218/.
Gurika GS, Gupta S, Kumar R. To determine the blood donor deferral pattern and its causes among blood donors in Tertiary Care Hospital. Int J Health Sci Res. 2024;14(8):428-34. doi: 10.52403/ijhsr.20240849.
Chauhan C, Chauhan R, Awasthi S, Dutta S, Joshi H. Pattern and outcome of donor deferral-need of hour. Int J Res Med Sci. 2017;6(1):289-92. doi: 10.18203/2320-6012.ijrms20175736.
Basavarajegowda A. Whole blood donor deferral causes in a Tertiary Care Teaching Hospital blood bank from South India. HTIJ. 2017;5(2):219-22. doi: 10.15406/htij.2017.05.00116.
Chauhan DN, Desai KN, Trivedi HJ, Agnihotri AS. Evaluation of blood donor deferral causes: a tertiary-care center-based study. Int J Med Sci Public Health. 2015;4(3):389-92. doi: 10.5455/ijmsph.2015.1211201470.
Ahmad N, Khan S, Hassan MJ, Jetley S. Analysis of blood donor deferral pattern in a new blood bank of a Tertiary Care Hospital in Delhi region. Int Arch Biomed Clin Res. 2020;6(1):PA7-PA11. doi: 10.21276/ddkrm204.
VS, RA, Haran AH, I SK, James S. Analysis of blood donor deferral pattern at a Tertiary Care Hospital in Chennai: a cross-sectional retrospective study. Cureus. 2024 Aug 22;16(8):e67541. doi: 10.7759/cureus.67541, PMID 39310487.
Saeed N, Akhtar A, Mudassar M, Danish M, Muzaffar A, Tariq TM. Blood donor deferral pattern and frequency at a Tertiary Care Hospital, Lahore. J Haematol Stem Cell Res. 2024;4(1):188-91.
Kujur DP, Tiwari DA, Bagde DS, Bombeshwar DV, Behera DT. Assessment of blood donor selection and deferral pattern in a Tertiary Care Hospital in Central India. Trop J Pathol Microbiol. 2020;6(1):83-8. doi: 10.17511/jopm.2020.i01.13.
Jain V, Kothari F. Analysis of blood donor deferral pattern at Tertiary Care Hospital. Int J Sci Res. 2021;10(8):78-80. doi: 10.36106/ijsr/1505647.
Singh J, Husain S, Giri V. Blood donor deferral pattern at Tertiary Care Teaching Institute in Western Uttar Pradesh, India. J Popul Ther Clin Pharmacol. 2023;30(17):1068-74.
Rajan RM, Anu J, Mathew AS. Profile of blood donors and deferral reasons in a Tertiary Care Centre in South India. J Adv Med Med Res. 2022;34(23):78-84. doi: 10.9734/jammr/2022/v34i234841.
Thivya DR, Vijayashree R, Meghanath K. Profile of blood donor deferrals in a tertiary care centre-our institutional experience. J Pharm Res Int. 2021;33(55B):75-80. doi: 10.9734/jpri/2021/v33i55B33848.
Unnikrishnan B, Rao P, Kumar N, Ganti S, Prasad R, Amarnath A. Profile of blood donors and reasons for deferral in coastal South India. Australas Med J. 2011;4(7):379-85. doi: 10.4066/AMJ.2011.641, PMID 23393523.
John F, Varkey MR. Evaluation of blood donor deferral causes in a Tertiary Hospital, South India. Int J Biomed Adv Res. 2015;6(3):253-8. doi: 10.7439/ijbar.v6i3.1833.