
Int J Curr Pharm Res, Vol 17, Issue 6, 82-87Original Article
COMPARING 0.75% ROPIVACAINE VS 0.5% LEVOBUPIVACAINE FOR SPINAL BLOCK IN PCNL SURGERIES: A RANDOMIZED STUDY
SHOWREDDY EDARA, HYMAVATHI V. N, V. VIJAY KUMAR REDDY, LAKKAM VAMSEE KIRAN*
Department of anesthesiology, RVM institute of medical sciences and research center, Siddipet, Telangana, India
*Corresponding author: Lakkam Vamsee Kiran; *Email: vamsee.lakkam@gmail.com
Received: 12 Aug 2025, Revised and Accepted: 02 Oct 2025
ABSTRACT
Objective: To evaluate the effectiveness, onset time, duration, and quality of both sensory and motor block, along with hemodynamic stability and postoperative pain relief, between 0.75% hyperbaric ropivacaine and 0.5% hyperbaric levobupivacaine during subarachnoid block in patients undergoing percutaneous nephrolithotomy (PCNL) procedures.
Methods: This prospective, randomized, observer-blinded study compared the efficacy of 0.75% hyperbaric ropivacaine and 0.5% hyperbaric levobupivacaine for subarachnoid block in 150 patients undergoing percutaneous nephrolithotomy (PCNL) surgeries. Patients were randomly allocated into two groups: Group R (n=75) received 4 ml of 0.75% hyperbaric ropivacaine, and Group l (n=75) received 4 ml of 0.5% hyperbaric levobupivacaine intrathecally. The onset and duration of the sensory and motor blockade, analgesia, perioperative hemodynamic variations, side effects, and complications were evaluated.
Results: Group l showed significantly earlier onset times for sensory (7.96±1.13 min vs. 9.99±2.57 min; P<0.0001) and motor blocks (2±0.62 min vs. 2.74±0.9 min; P<0.0001) compared to Group R. The duration of sensory block (83.33±10.18 min vs. 59.57±8.15 min), analgesia (145.49±7.93 min vs. 127.8±6.22 min), and motor block (287.25±40.72 min vs. 199±24.38 min) were significantly longer in Group l (P<0.0001). The hemodynamic parameters remained stable in both groups, with no significant differences between the groups. The incidence of side effects was comparable between the groups.
Conclusion: In conclusion, 0.5% hyperbaric levobupivacaine provides a faster onset and prolonged duration of sensory and motor blockade, as well as extended analgesia, compared to 0.75% hyperbaric ropivacaine for subarachnoid block in PCNL surgeries, with a similar safety profile.
Keywords: Ropivacaine, Levobupivacaine, PCNL Surgeries, Subarachnoid block
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i6.7095 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) is the gold standard treatment for renal calculi, particularly when extracorporeal shockwave lithotripsy (ESWL) has limitations. Fernstrom and Johansson first described this minimally invasive method of renal stone removal in 1976 [1]. General, spinal, or epidural anesthesia may be used for this procedure [2, 3].
Spinal anesthesia has a number of benefits over general anesthesia, such as less postoperative pain, quicker recovery period, and lower incidence of complications, and is becoming a more popular regional anesthesia technique for percutaneous nephrolithotomy (PCNL) surgeries [3, 4].
Overview of hyperbaric ropivacaine and levobupivacaine
Choosing an ideal local anesthetic for spinal anesthesia during PCNL is crucial. Levobupivacaine and ropivacaine are local anesthetics used in various surgical procedures, particularly spinal and epidural anesthesia.
Ropivacaine is a pure S(–)enantiomer, a long-acting local anesthetic used for pain management and surgery. It is safer than bupivacaine for regional anesthesia and pain management following surgery because it is less toxic and has fewer side effects [5, 6].
Levobupivacaine is a long-acting amino-amide local anesthetic that shares structural similarities with bupivacaine, the S-enantiomer of bupivacaine, and it exhibits comparable anesthetic and analgesic properties. It is recommended as a safer option for racemic bupivacaine in clinical situations where the threat of toxicity is heightened owing to its favorable side-effect profile [7].
Ropivacaine and levobupivacaine are increasingly used in a variety of surgical settings to improve patient safety and provide efficient pain relief [8]. Both levobupivacaine and ropivacaine are available in hyperbaric formulations, allowing for controlled distribution in the subarachnoid space and consistent anesthesia. According to earlier research, levobupivacaine has a potency ratio of 1:1.5, compared to ropivacaine [9, 10]. For PCNL surgeries, levobupivacaine was utilized at 20 mg (5 mg per ml) to compare with ropivacaine at 30 mg (7.5 mg per ml) to guarantee adequate sensory and motor block.
Study design: randomized observer-blind methodology
This prospective, randomized, comparative study was conducted between June 2022 and June 2023.
Patient selection criteria and ethical considerations
Following approval from the institutional ethics committee, written informed consent was obtained from either the patient or their designated guardian.
Inclusion criteria
A total of 150 patients of both sexes, aged between 18 and 70 y and classified as American Society of Anesthesiologists (ASA) class I and II, who were scheduled for percutaneous nephrolithotomy surgery, were enrolled in the study.
Exclusion criteria
Patients classified as ASA III or above, those who refused participation, individuals with allergies to the study medications, patients with coagulation disorders, infections at the injection site, spinal deformities, neurological disorders, and significant hypovolemia were excluded. The patients were randomized into two groups at a ratio of 1:1, each comprising 75 participants. Group l was administered intrathecal hyperbaric levobupivacaine 0.5% (4 ml), whereas Group R received intrathecal hyperbaric ropivacaine 0.75% (4 ml).
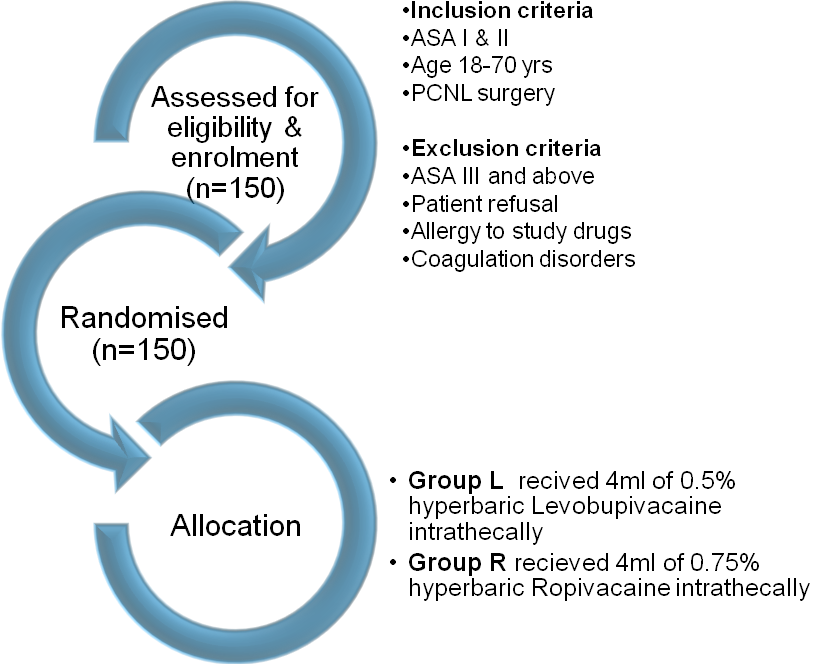
Fig. 1: Schematic reforestation of the study
A pre-anesthesia check-up was conducted the day before surgery for all patients, and written informed consent was obtained for both the study and spinal anesthesia. Patients were kept nil by mouth for 8 h before surgery and given 0.5 mg alprazolam at bedtime prior to the procedure. On the day of surgery, patients were re-examined and re-assessed. An intravenous 18G cannula was established, and 15 ml/kg of lactated Ringer’s solution was administered 30 min before the procedure. Patients were then moved to the operating room, where a multiparameter monitor was attached to record baseline parameters, such as heart rate, oxygen saturation, non-invasive blood pressure, and electrocardiogram, throughout the procedure.
Patients were divided into two groups: 150 patients planned for elective PCNL surgeries under subarachnoid block of either sex were randomized as, Group R (N=75), that is, Ropivacaine heavy 0.75% group. Group l (N=75) i. e. Levobupivacaine heavy 0.5% group
Blinding
The study medication was prepared in identical 5 ml syringes by an uninvolved person to ensure blinding of the anesthetist. The observations were conducted by a single investigator who was blinded to the study drug. Subarachnoid block was performed with the patient in a sitting position, using strict aseptic techniques. A lumbar puncture was performed at the L3-L4 intervertebral space with a 25-gauge Quincke spinal needle to confirm the free flow of cerebrospinal fluid. Patients in group R received 4 ml of 0.75% hyperbaric ropivacaine, whereas those in group l received 4 ml of 0.5% hyperbaric levobupivacaine. After the injection, the patients were positioned supine. Hemodynamic parameters, including heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP), were recorded immediately after the injection and subsequently at intervals of 2 min for the first 15 min, then every 5 min up to 30 min, and every 15 min up to 90 min, regardless of the study duration.
Comparative analysis of 0.75% ropivacaine vs. 0.5% levobupivacaine
This study aimed to evaluate the onset and duration of sensory and motor blockade and analgesia as primary objectives, while assessing perioperative hemodynamic variations, side effects, and complications as secondary objectives.
The findings from this comparative analysis will provide valuable insights into the efficacy and safety profiles of these two local anesthetics, potentially guiding clinical decisions in regional anesthesia practices.
Outcome measures
Assessing anesthetic efficacy following parameters were recorded. The onset of sensory block was measured by the loss of sensation to the pin prick at the T6 dermatome, while motor blockade onset was assessed using the modified Bromage scale, with grade 3 indicating complete motor block. The quality of motor blockade is categorized into four grades: grade 0 (no motor block), grade 1 (inability to raise the extended leg but able to move the knees and feet), grade 2 (inability to raise the extended leg and move the knee, but able to move the feet), and grade 3 (complete motor block). The duration of sensory blockade was evaluated using two-segment regression, and the duration of motor blockade was measured from the onset of complete motor block (Bromage grade 3) to complete motor recovery. Analgesia duration was noted when the patient reported pain, with a visual analog scale score of 5.
Intraoperative monitoring included non-invasive blood pressure (NIBP), ECG, and pulse oximeter. Heart rate and blood pressure (SBP, DBP, and MAP) were recorded immediately after drug injection and subsequently every 2 min for the first 15 min, then every 5 min up to 30 min, and every 15 min until 90 min. Patients were monitored for adverse effects, such as inadequate block, hypotension (decrease in systolic blood pressure by 20% from baseline or any value below 90 mmHg), bradycardia (heart rate<60 bpm), respiratory distress, nausea, vomiting, and anaphylactic reactions. Treatment for hypotension included rapid intravenous fluid infusion, oxygen inhalation, elevation of the legs, and administration of intravenous Ephedrine and Atropine for the associated bradycardia. Nausea and vomiting were managed using ondansetron.
Statistical methods for data analysis
This study was a prospective, randomized, observer-blind trial involving randomly selected patients. Data entry and analysis were performed using Microsoft Excel 2020 and SPSS version 22, respectively, employing both descriptive and inferential statistical methods. Continuous variables were reported as mean±SD deviation, and categorical data as number (%). Demographic data were assessed using the student’s t-test or Chi-square test, with quantitative data analyzed using the student’s t-test and qualitative data using the Chi-square test. Statistical significance was set at P<0.05.
RESULTS
The study found that demographic characteristics such as age, sex, weight, and height were comparable between the two groups, with no statistically significant differences. The mean age was 41.3±13 y for group R and 42±11.5 y for group L(p=0.58). The sex distribution was as follows: 57 males and 18 females in group R, and 54 males and 21females in group L. The mean weight was 58.46±5.6 kg for group R and 60.3±10.3 kg for group l (p=0.17). The mean height was 162±7.3 cm in group R and 163±7.5 cm in group l (p=0.29). Statistical analysis was performed using the student’s t-test, with significance set at P<0.05.
Table 1: Comparison of demographic characteristics between the two groups
| Characteristics | Group R | Group L | P value |
| Mean age in years (mean±SD) | 41.3 ±13 | 42±11.5 | 0.58 |
| Sex (number of males/number of females) | 57/18 | 54/21 | |
| Weight in kg (mean±SD) | 58.46±5.6 | 60.3±10.3 | 0.17 |
| Height in cm (mean±SD) | 162±7.3 | 163±7.5 | 0.29 |
Table 2: Comparison of block characteristics between the two groups
| Characteristics | Group R mean±SD | Group L mean±SD | P value |
| Time for onset of sensory block (min) | 9.99±2.57 | 7.96±1.13 | <0.0001 |
| Time for onset of motor block (min) | 2.74±0.9 | 2±0.62 | <0.0001 |
| Duration of sensory block (min) | 59.57±8.15 | 83.33±10.18 | <0.0001 |
| Duration of analgesia (min) | 127.8±6.22 | 145.49±7.93 | <0.0001 |
| Duration of motor block (min) | 199±24.38 | 287.25±40.72 | <0.0001 |
Value are expressed as mean (SD), P<0.05, significant, SD Standard deviation.
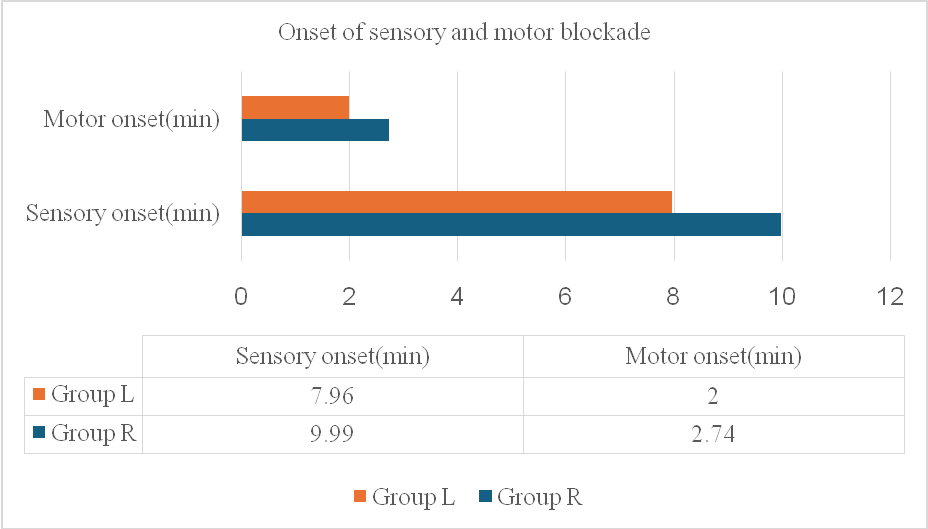
Fig. 2: Comparison of onset of sensory and motor blockade
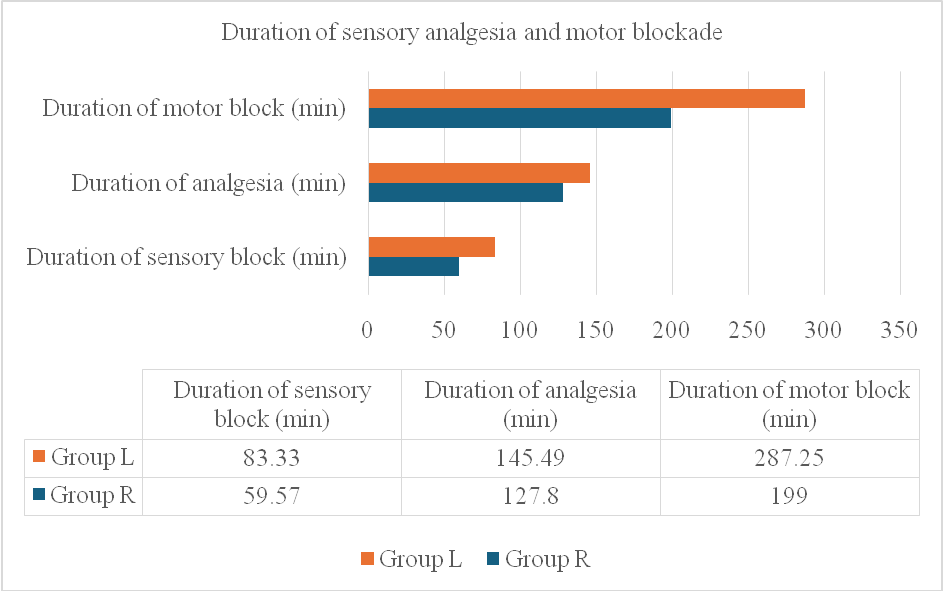
Fig. 3: Comparison of duration of sensory blockade, analgesia and motor blockade
This study compared the effects of 0.5% heavy levobupivacaine and 0.75% heavy ropivacaine on sensory and motor block characteristics. Group l (Levobupivacaine) showed significantly earlier onset times for both sensory (7.96 min vs. 9.99 min) and motor blocks (2 min vs. 2.74 min), with P<0.0001. Additionally, the duration of sensory block (83.33 min vs. 59.57 min), analgesia (145.49 min vs. 127.86 min), and motor block (287.25 min vs. 199.24 min) were longer in group L, all statistically significant (P<0.001). The baseline hemodynamic parameters were similar between the groups, with no significant changes over time. Both groups had equal incidences of bradycardia (2.60%) and vomiting (2.60%), whereas hypotension occurred in 8% of the ropivacaine group and 6.66% of the levobupivacaine group, which was not statistically significant. Overall, both anesthetics displayed comparable safety profiles with regard to side effects.
Discussion of results: implications for clinical practice
Percutaneous nephrolithotomy (PCNL) has been established as a pivotal surgical technique for the management of large and complex kidney stones, offering a minimally invasive alternative that presents numerous benefits for patients. The success of PCNL is significantly contingent on the selection of appropriate anesthesia, which is essential for ensuring patient comfort, effective pain management, and the creation of optimal conditions for the surgical procedure. Among the various anesthetic options available, spinal anesthesia is the preferred choice. This technique involves the subarachnoid injection of local anesthetic agents, which induces profound sensory and motor blockade while simultaneously providing postoperative analgesia. Selection of the most suitable local anesthetic for spinal anesthesia during PCNL is of paramount importance.
Two long-acting local anesthetics that are frequently used in this context are Ropivacaine and Levobupivacaine. These agents are considered safer alternatives to traditional anesthetics, such as bupivacaine, primarily because of their lower risk profiles.
Ropivacaine, an amide-type local anesthetic, is associated with a diminished risk of cardiotoxicity and central nervous system toxicity, making it a favorable option in clinical practice. Levobupivacaine, which is the S-enantiomer of bupivacaine, shares these advantages, further enhancing its safety profile. Both Ropivacaine and Levobupivacaine are available in hyperbaric formulations, which facilitate controlled distribution within the subarachnoid space, thereby ensuring reliable and consistent anesthesia during surgical procedures.
The present study was designed to compare the efficacies of 0.75% hyperbaric ropivacaine and 0.5% levobupivacaine in patients undergoing PCNL surgeries. Demographically, the mean age of participants in Group R was recorded at41.39±13 y, while Group l had a mean age of 42±11.05 y. These demographic data indicate that age was comparable across both groups, with an age range spanning from 18 to 70 y, consistent with findings from previous studies, including those of Mehta [10] and Athar [11], and Charan H [12]. In terms of sexdistribution, Group R comprised 57 males and 18 females, whereas Group l included 54 males and 21 females. This sex distribution was comparable to that observed in other studies, reinforcing the validity of the findings. The average weight of participants in Group R was 58.46±5.62 kg, while Group l exhibited an average weight of 60.33±10.36 kg. These mean weights were consistent with those reported in earlier studies by Mehta A [10]. (59.76±6.49 kg and 59.56±7.98 kg) and Athar [11]. (57.17±6.65 kg and 53.83±9.44 kg). Furthermore, the average height in Group Rwas measured at 162.64±7.31 cm, compared to 163.9±7.50 cm in Group L. The mean heights of the participants in this study were also comparable to those reported in the literature, including Mehta A [10]. (173.36±8.68 cm and170±7.61 cm) and Charan H [12]. (161.21±7.15 cm and 163.50±6.37 cm). Overall, these findings indicate that both groups exhibited similar physical characteristics, suggesting a balanced distribution of participants in terms of weight and height. This homogeneity is crucial for the validity and reliability of the study outcomes, as it minimizes the potential for confounding variables that could influence the comparative efficacy of the anesthetic agents being studied.
An essential factor to consider when evaluating the efficacy of anesthetics is the onset of the sensory blockade. Our study demonstrated that levobupivacaine significantly outperformed ropivacaine in terms of achieving a faster sensory blockade. Specifically, the average time required for the onset of sensory blockade was notably shorter with levobupivacaine, recorded at 7.96±1.13 min, compared to ropivacaine, which took 9.99±2.57 min. This finding aligns with the previous research conducted by Mehta [10], Athar [11], and Dr. Alpa M Patel [13], all of whom reported a markedly quicker onset of sensory blockade with levobupivacaine than with ropivacaine. Forinstance, Mehta [10] discovered that the onset time of levobupivacaine was 4.38 min, whereas that of ropivacaine was 5.45 min. Athar [11] reported durations of 13.50 and 7.33 min for ropivacaine and levobupivacaine, respectively. Similarly, Dr. Alpa M Patel [13], observed an onset of 3.47 min for Levobupivacaine when compared to 5.82 min for Ropivacaine. Conversely, Sagar. [14] showed no significant difference in onset times between the two anesthetics, with Levobupivacaine averaging 3.85±0.5 min and Ropivacaine at 3.90±0.6 min. Charan [12], Gurpreet [15] reported comparable onset times, with Charan [12] reporting 2.91±0.91 min for Levobupivacaine and 2.51±1.31 min for Ropivacaine, while Gurpreet [15] found mean onset times of 15.5±1.81 min for Levobupivacaine and 17.07±1.81 min for Ropivacaine. These varying results underscore a general trend favoring Levobupivacaine for achieving a quicker sensory blockade, although some studies did not find significant differences.
In terms of motor onset, our study also indicated that Levobupivacaine had a s faster onset time of 2±0.62 min compared to Ropivacaine, which took 2.74±0.9 min. This finding is consistent with those reported results by of Mehta [10], who reported a motor onset of 5.46±1.72 min for levobupivacaine versus 6.46±1.14 min for ropivacaine. Dr. Alpa M Patel [13] further corroborated this trend, noting a motor onset of 1.68±0.63 min for levobupivacaine compared to 2.82±0.62 min for Ropivacaine. In contrast however, Athar [11] reported a contrasting finding, indicating a longer motor onset time for levobupivacaine at 12.17±4.09 min compared to 7.83±2.84 min for Ropivacaine. Conversely, three studies Charan [12], Sagar [14], and Gurpreet [15], found no significant differences in the motor onset times between the two anesthetics. Charan [12], recorded times of 3.56±0.99 min for ropivacaine and 3.65±1.01 min for levobupivacaine, while Sagar [14], reported 3.82±0.88 min for ropivacaine and 3.65±0.72 min for levobupivacaine. Gurpreet [15] also noted comparable durations, with ropivacaine averaging 25.07±1.97 min and levobupivacaine at 24.37±1.70 min. Overall, the findings from our study, along with the existing literature, suggest that levobupivacaine often provides a faster onset of both sensory and motor blockade than compared to ropivacaine, although some studies indicate variability in these outcomes.
Our comprehensive study revealed a noteworthy extension in the duration of sensory block when utilizing Levobupivacaine, averaging 83.33±7.93 min, in comparisonto Ropivacaine, which averaged 59.57±8.15 min. These findings are consistent in line with those of a multitude of studies in the field. For instance, Mehta A [10] observed a significantly prolonged sensory block duration with Levobupivacaine (189.4±42.9 min) compared to Ropivacaine (144.32±32.1 min). Similarly, Athar [11] reported an even more pronounced difference, with Levobupivacaine achieving a sensory block duration of 251.50±33.12 min versus ropivacaine 191.50±22.86 min. Furthermore, Dr. Alpa M Patel [13] corroborated these results, indicating that levobupivacaine (101.91±11.84 min) significantly outlasted Ropivacaine (94.18±7.74 min). Gurpreet [15] also noted a significant difference, with levobupivacaine providing a sensory block duration of 69±8.5 min compared to ropivacaine's 61.83±6.31 min. However, it is worth mentioning that the Sagar [14] reported no statistically significant difference in sensory block duration, with Levobupivacaine averaging 98.27±10.18 min and Ropivacaine 96.33±8.21 min.
In terms of analgesia, our study demonstrated a significantly longer duration with Levobupivacaine (145.49±7.93 min) than compared with to Ropivacaine (127.8±16.223 min). This observation aligns with previous research, such as that by Athar [11], who noted a substantial increase in analgesic duration with Levobupivacaine (309.83±36.45 min) compared to ropivacaine (249.50±22.86 min). In additionally, Dr. Alpa M Patel [13] reported similar findings, emphasizing the extended analgesic effect of Levobupivacaine. Conversely, Sagar [14] found no significant difference in analgesia duration, reporting Levobupivacaine at 262.22±36.60 min and Ropivacaine at 261.20±32.71 min, highlighting some variability in the literature. Moreover, our study indicated a significant prolongation in the duration of motor blockade with Levobupivacaine (287.25±40.72 min) compared to that with ropivacaine (199±24.38 min). This is consistent with findings from other studies, such as Mehta A [10], who reported a motor blockade duration of 172.76±38.9 min for levobupivacaine versus 128.24±29.1 min for Ropivacaine. Similarly, Athar [11] found a longer motor blockade duration with levobupivacaine (290.5±34.67 min) compared to Ropivacaine (222.50±23 min). Dr. Alpa M Patel [13] also corroborated these findings, reporting a significant difference with Levobupivacaine (183±10.59 min) outlasting Ropivacaine (154±9.61 min). However, not all studies concurred with these results, such as those of like Charan H [12] found no significant difference in motor blockade duration (Levobupivacaine: 141.21±7.15 min; Ropivacaine: 152±7.15 min), and Sagar [14] also reported similar findings (Levobupivacaine: 201.15±22.06 min; Ropivacaine: 204±21.20 min). Gurpreet [15] further noted no significant difference in motor blockade duration (Levobupivacaine: 116.73±29.95 min; Ropivacaine: 112.93±15.40 min). Importantly, our study demonstrated that both Levobupivacaine and Ropivacaine maintained stable hemodynamic parameters throughout the surgical procedures, with no significant differences observed between the two groups. This finding is consistent with those the results reported by Mehta [10], who noted that both anesthetics provided stable hemodynamic profiles in patients undergoing lower limb surgeries. Similarly, Sagar [14] observed comparable hemodynamic stability in their study.
Key observations from the study highlight several advantages of using 0.5% hyperbaric levobupivacaine
Accelerated Onset of Sensory Blockade: The administration of 0.5% hyperbaric levobupivacaine significantly shortens the time required for the sensory blockade to take effect, allowing for faster patient comfort and readiness for surgical intervention.
Rapid Onset of Motor Blockade: This formulation also facilitates a quicker onset of motor blockade, which is crucial in surgical settings where prompt immobilization of the patient is necessary.
Prolonged Sensory Blockade: One of the most noteworthy benefits is the extended duration of sensory blockade provided by 0.5% hyperbaric levobupivacaine, which ensures prolonged pain relief throughout the surgical procedure and into the postoperative recovery phase.
Extended Motor Blockade Duration: In addition to a rapid onset, this anesthetic agent offers a longer-lasting motor blockade, which can enhance surgical conditions and patient safety.
Stable Hemodynamic Profile: Importantly, the use of 0.5% hyperbaric levobupivacaine was associated with no significant hemodynamic changes, ensuring that the blood pressure and heart rate remained stable throughout the procedure.
Lower Risk of Complications: The study indicates that this anesthetic does not increase the likelihood of common complications, such as bradycardia, hypotension, nausea, or vomiting, which are often associated concerns with spinal anesthesia.
While both 0.75% hyperbaric ropivacaine and 0.5% levobupivacaine are viable options for spinal anesthesia, the evidence strongly supports the preference for levobupivacaine because due to its superior profile in terms of anesthesia quality, pain relief, and safety. This, positions 0.5% hyperbaric levobupivacaine as a highly effective choice for clinicians seeking to optimize patient outcomes during PCNL surgeries. In conclusion, the choice of anesthetic plays a crucial role in enhancing patient safety and comfort, making it imperative for clinicians to consider these findings when planning surgical interventions.
LIMITATIONS OF THIS STUDY
The study was limited by its sample size and the specific patient demographics, which may not fully represent the broader population undergoing PCNL surgeries. Future research should aim to include a more diverse patient population and larger sample sizes to validate these findings and further explore the long-term outcomes associated with different anesthetic agents in PCNL procedures. These efforts will not only improve the quality of care provided to patients but also contribute to the ongoing evolution of best practices in anesthetic management during urological surgeries.
CONCLUSION
Based on the findings of this study, we can draw significant conclusions regarding the efficacy and safety of 0.5% hyperbaric levobupivacaine when administered intrathecally, particularly in the context of percutaneous nephrolithotomy (PCNL) surgeries. The results suggest that this 0.5% hyperbaric levobupivacaine not only enhances anesthesia and pain management but also minimizes the incidence of adverse effects, while maintaining stable hemodynamic parameters, especially in comparison to the 0.75% hyperbaric ropivacaine.
Declaration of patient consent
The authors attested that all the necessary patient consent forms have been obtained. The patients have provided writtentheir consent in writing for their pictures and other medical data to be published in the journal. The patients are aware that although every attempt will be made to hide their identities, anonymity cannot be ensured. Their names and initials will notbe published.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors contributed equal
CONFLICTS OF INTEREST
There are no conflicts of interest
REFERENCES
Fernstrom I, Johansson B. Percutaneous pyelolithotomy: a new extraction technique. Scand J Urol Nephrol. 1976;10(3):257-9. doi: 10.1080/21681805.1976.11882084, PMID 1006190.
Cicek T, Gonulalan U, Dogan R, Kosan M, Istanbulluoglu O, Gonen M. Spinal anesthesia is an efficient and safe anesthetic method for percutaneous nephrolithotomy. Urology. 2014 Jan;83(1):50-5. doi: 10.1016/j.urology.2013.08.064, PMID 24210569.
Malik I, Wadhwa R. Percutaneous nephrolithotomy: current clinical opinions and anesthesiologists' perspective. Anesthesiol Res Pract. 2016;2016:9036872. doi: 10.1155/2016/9036872, PMID 27110239, PMCID PMC4826713.
Mehrabi S, Karimzadeh Shirazi K. Results and complications of spinal anesthesia in percutaneous nephrolithotomy. Urol J. 2010;7(1):22-5. PMID 20209451.
Simpson D, Curran MP, Oldfield V, Keating GM. Ropivacaine: a review of its use in regional anaesthesia and acute pain management. Drugs. 2005;65(18):2675-717. doi: 10.2165/00003495-200565180-00013, PMID 16392884.
Olapour A, Akhondzadeh R, Rashidi M, Gousheh M, Homayoon R. Comparing the effect of bupivacaine and ropivacaine in Cesarean delivery with spinal anesthesia. Anesthesiol Pain Med. 2020 Jan 18;10(1):e94155. doi: 10.5812/aapm.94155, PMID 32337166, PMCID PMC7144247.
Weinberg L, Hu R, Chen S. Levobupivacaine for regional anesthesia and pain management. Clinical Medicine Reviews in Therapeutics. 2011;S5150. doi: 10.4137/cmrt.s5150.
Casati A, Putzu M. Bupivacaine, levobupivacaine and ropivacaine: are they clinically different? Best Pract Res Clin Anaesthesiol. 2005 Jun;19(2):247-68. doi: 10.1016/j.bpa.2004.12.003, PMID 15966496.
Parpaglioni R, Frigo MG, Lemma A, Sebastiani M, Barbati G, Celleno D. Minimum local anaesthetic dose (MLAD) of intrathecal levobupivacaine and ropivacaine for Caesarean section. Anaesthesia. 2006 Feb;61(2):110-5. doi: 10.1111/j.1365-2044.2005.04380.x, PMID 16430561.
Mehta A, Gupta V, Wakhloo R, Gupta N, Gupta A, Bakshi R. Comparative evaluation of intrathecal administration of newer local anaesthetic agents ropivacaine and levobupivacaine with bupivacaine in patients undergoing lower limb surgery. Internet J Anesthesiology. 2007;17(1).
Athar M, Moied Ahmed S, Ali S, Doley K, Varshney A, Hussain Siddiqi MM. Levobupivacaine or ropivacaine: a randomised double blind controlled trial using equipotent doses in spinal anaesthesia. Colomb J Anesthesiology. 2016 Apr 1 44(2):97-104.
Hansraj Charan, Pravin Dhone. Comparison between levobupivacaine and ropivacaine for spinal anaesthesia. Global Journal for Research Analysis. 2019 Jul;8(7).
Patel DA. Effectiveness of ropivacaine versus levobupivacaine for spinal anaesthesia and analgesia in lower limb surgery. JMSCR. 2018;6(2):930-7. doi: 10.18535/jmscr/v6i2.144.
Byndoor Y, Sagar TV. Levobupivacaine versus ropivacaine in patients undergoing lower abdominal surgeries. Indian J Pharm Pharmacol. 2023;10(2):111-5. doi: 10.18231/j.ijpp.2023.023.
Singh G, Rathod NM, Patel K. Comparison of equipotent doses of Hyperbaric Ropivacaine and hyperbaric levobupivacaine in spinal anaesthesia for patients undergoing lower abdominal and lower limb surgeries. Indian J Anaesthesia and Anagesia. 2019:6(1):249-54. doi: 10.21088/ijaa.2349.8471.6119.35.