
Int J Curr Pharm Res, Vol 17, Issue 6, 92-96Original Article
HISTOPATHOLOGICAL SPECTRUM OF GASTROINTESTINAL LESIONS: CORRELATING BIOPSY WITH ENDOSCOPY FINDINGS
BHARADWAJ VEDULA*, THALLURY SHIRIN KAMAL, G. RAJA PRAMILA
Department of Pathology, Gitam Institute of Medical Sciences and Research, Visakhapatnam, India
*Corresponding author: Bharadwaj Vedula; *Email: alzheimers88@gmail.com
Received: 12 Aug 2025, Revised and Accepted: 02 Oct 2025
ABSTRACT
Objective: To assess the spectrum of histopathological findings in gastrointestinal (GI) lesions and correlate them with endoscopic impressions to evaluate diagnostic accuracy and concordance.
Methods: This retrospective observational study was conducted in the Department of Pathology at a tertiary care center from January 2021 to March 2024. A total of 76 endoscopic GI biopsy samples were analyzed after applying inclusion and exclusion criteria. Endoscopic features were documented from requisition forms and compared with corresponding histopathological diagnoses. Sensitivity, specificity, predictive values, and diagnostic concordance were calculated, and statistical analysis was performed using the Chi-square test and Cohen’s Kappa.
Results: Out of 76 cases, 55 (72.3%) were non-neoplastic and 21 (27.6%) were neoplastic. The most common non-neoplastic diagnosis was non-specific inflammation (38.2%), while carcinoma was the predominant neoplastic lesion (76.2% of neoplastic cases). Endoscopic growths were most predictive of malignancy, while mucosal changes and ulcerations were often associated with benign conditions. Endoscopy showed a sensitivity of 80.9%, specificity of 72.7%, and diagnostic accuracy of 75% in identifying neoplastic lesions. The concordance rate between endoscopic and histopathological findings was 67%, with a Cohen’s Kappa value of 0.67, indicating substantial agreement.
Conclusion: Endoscopy remains a valuable initial diagnostic tool, but histopathological confirmation is essential, especially for distinguishing benign from malignant GI lesions. This study highlights the importance of integrating both modalities to improve diagnostic confidence and guide appropriate clinical management.
Keywords: Biopsy, Colon, Endoscopy, Gastrointestinal, Histopathology, Inflammation, Lesions
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i6.7098 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Gastrointestinal (GI) disorders are some of the most common issues seen in clinical settings and present a wide spectrum of symptoms ranging from mild discomfort to life-threatening complications [1]. A definitive diagnosis is crucial for guiding appropriate management and improving patient outcomes.
Endoscopy is now an essential procedure for the initial assessment of gastrointestinal disorders, as it provides direct visualization of the mucosal lining and allows for biopsy collection from the suspicious lesions [2]. However, endoscopic impressions alone can sometimes be misleading, as lesions that appear benign may harbor underlying malignancy. At the same time, some suspicious-looking findings may turn out to be inflammatory or reactive on biopsy [3, 4].
Endoscopic findings are most reliably confirmed through histopathological evaluation of biopsy samples. In addition to enhancing diagnostic accuracy, this method helps in the detailed classification of lesions, better assessment of disease progression, and earlier detection of neoplastic transformations [5]. Integrating clinical data with endoscopic observations and histopathological results significantly improves diagnostic precision.
In this study, we aim to characterize the histopathological spectrum of upper and lower GI lesions obtained via endoscopic biopsies, assess their distribution and frequency across different anatomical sites of the GI tract, correlate the histopathological findings with endoscopic features, and analyze the degree of concordance between the endoscopic findings and histopathological diagnoses. Understanding this correlation is essential in strengthening diagnostic confidence and optimizing the management of gastrointestinal diseases.
MATERIALS AND METHODS
This is a cross-sectional observational retrospective study conducted in the department of Pathology at a tertiary care hospital from January 2021 to March 2024. All endoscopic gastrointestinal biopsies received during this period were included in the study following the inclusion and exclusion criteria. Inadequate tissue samples and tissue submitted that was not from the representative area are excluded from the study. Specimens were fixed in neutral buffered formalin, routinely processed, and examined with H and E stain. Special stains such as PAS and Giemsa were applied as and when required. Clinical data was retrieved from requisition forms, including history, endoscopic findings, and clinical diagnosis, and analysed. Institutional ethics committee approval was also obtained-IEC 327/2024.
RESULTS
Eighty cases of gastrointestinal biopsies were received during the study period, of which 76 cases met the inclusion criteria and were analysed. The age of the patients ranged from 8 to 75 y (fig. 1). There were 34 females (45%) and 42 males (55%) with a male-to-female ratio of 1.23:1 (fig. 2).
As shown in table 1, the anatomical distribution of endoscopic biopsy specimens demonstrated a predominance of cases involving the colon and rectum (29 cases, 38.15%), followed by the stomach (22 cases, 28.94%). In contrast, the ileum and ileocolic junction represented the least frequently sampled sites, each accounting for 2 cases (2.63%).
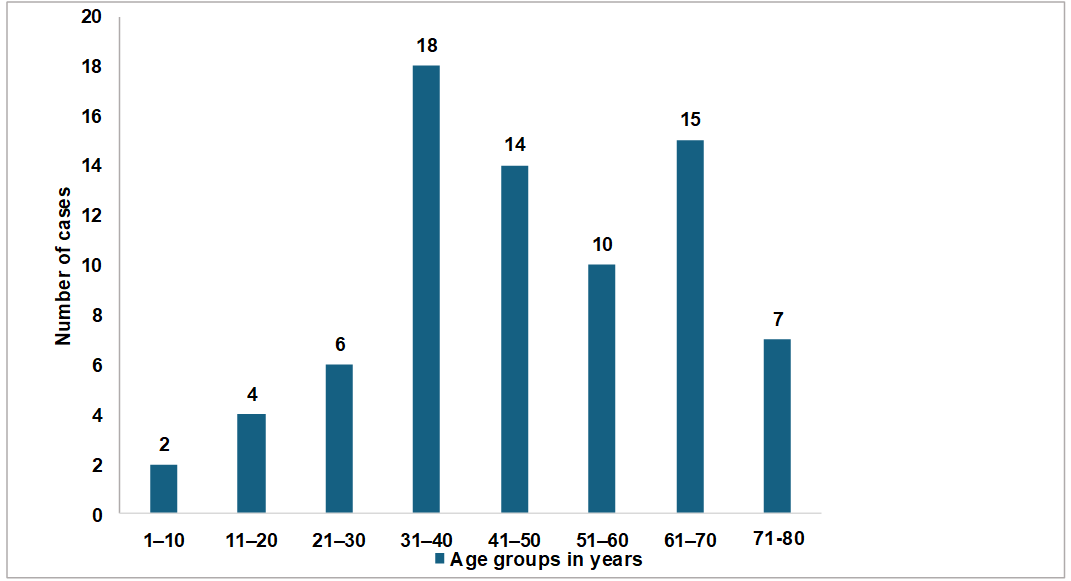
Fig. 1: Age wise distribution of cases
Fig. 2: Sex distribution of cases
Table 1: Site-wise distribution of cases (n-76)
| Site | No. of cases |
| Esophagus | 3(3.94%) |
| Gastroesophageal junction | 3 (3.94%) |
| Stomach | 22 (28.94%) |
| Duodenum | 15 (19.73%) |
| Ileum | 2 (2.63%) |
| Colon and Rectum | 29 (38.15%) |
| Ileocolic junction | 2 (2.63%) |
Histopathological Diagnosis
Of the 76 cases analyzed, 55 (72.3%) were classified as non-neoplastic, while 21 (27.63%) were identified as neoplastic. Non-specific inflammation was the predominant finding among the non-neoplastic lesions, observed in 21 cases (27.63%). Within the neoplastic category, carcinomas were the most prevalent, comprising 16 cases (76.19%), followed by polyps, which accounted for 3 cases (14.2%) (table 2).
Endoscopic findings
Table 3 outlines the endoscopic findings for each case. The most common endoscopic findings included mucosal changes (edema, erythema, scalloping, erosion) observed in 19 cases (25%), while normal mucosa was noted in 7 cases (9.21%).
Correlation of endoscopic features with histopathology
Among the 76 cases, non-neoplastic findings were more diverse, with 19 (25%) showing mucosal changes and 18 (23.68%) presenting ulceration or erosion. In contrast, neoplastic cases predominantly showed growth, with 14 (18.42%) cases demonstrating this feature. Polyps were more commonly seen in non-neoplastic cases (n-13, 17.1%), while only 3 (3.9%) of neoplastic cases had polyps. Overall, mucosal changes and normal findings were more prevalent in non-neoplastic cases, while growth was more frequently observed in neoplastic cases (table 4).
Statistics
Endoscopic features were grouped into “suspicious” (growth and polyp) and “non-suspicious” (ulcer/erosion, mucosal changes, normal) categories to evaluate their correlation with histopathological diagnosis. Using this classification, endoscopy demonstrated a sensitivity of 80.9%, specificity of 72.7%, positive predictive value of 53%, and negative predictive value of 90% in detecting neoplastic lesions. A Chi-square test revealed a statistically significant association between endoscopic findings and histopathology (χ² = 18.15, degrees of freedom = 1, p<0.0001), indicating that suspicious endoscopic features strongly correlated with neoplastic biopsy results.
The accuracy of endoscopy was 75% indicating that endoscopy correctly identified both neoplastic and non-neoplastic lesions in 75% of cases. A Cohen’s Kappa of 0.67 indicates a substantial agreement between the endoscopic findings and histopathological diagnosis.
Table 2: Histopathological diagnosis (n-76)
| Non-neoplastic | n-55 (72.3%) |
| Tuberculosis | 1 (1.81%) |
| Crohn`s disease | 2 (3.63%) |
| Ulcerative colitis | 1 (1.81%) |
| Malabsorption | 3 (5.45%) |
| Gastritis | 5 (9.09%) |
| ulcer | 4 (7.27%) |
| Non-specific inflammation | 21 (38.18%) |
| Brunner gland hyperplasia/adenoma | 5 (9.09%) |
| Peptic duodenitis | 3 (5.45%) |
| Polyps | 10 (18.18%) |
| Neoplastic | n-21 (27.63%) |
| Polyp | 3 (14.28%) |
| Dysplasia | 2 (9.5%) |
| Carcinoma | 16 (76.19%) |
Table 3: Endoscopic findings (n-76)
| Ulcer | 18 (23.68%) |
| Growth | 16 (21.05%) |
| Polyp | 16(21.05%) |
| Mucosal changes (edema, erythema, scalloping, erosion) | 19 (25%) |
| Normal | 7 (9.21%) |
Table 4: Endoscopic presentation and histopathological findings
| Endoscopic features | Non-neoplastic in biopsy (n-55) | Neoplastic in biopsy (n-21) | Total (n-76) |
| Ulcer/erosion | 16 | 2 | 18 |
| Growth | 2 | 14 | 16 |
| Polyp | 13 | 3 | 16 |
| Mucosal changes | 17 | 2 | 19 |
| Normal | 7 | 0 | 7 |
DISCUSSION
Lesions of the gastrointestinal tract are commonly diagnosed in medical practice and are categorized based on their anatomical position into those affecting the upper or lower segments of the GI system. Using both biopsy and endoscopy together is essential when diagnosing gastrointestinal (GI) issues as this combination not only leads to a more accurate diagnosis but also aids in tracking the progression of these conditions. Many GI lesions that look suspicious on endoscopy are now being sampled and sent for histopathological examination, resulting in early identification of these lesions.
This study analyzed 76 endoscopic biopsy samples from both the upper and lower gastrointestinal tract over three years. Patient ages ranged from 8 to 75 y, with the highest incidence observed in the 31–40 age group (n = 14, 18.42%), followed closely by the 61–70 y group (n = 15, 19.73%). The lowest cases were recorded in the 1–10 age group (n = 2, 2.6%). Most of the cases were in the 31-60 y age group (n-42, 55.26%) as seen in other studies [6-9]. This study showed that GI lesions were more common in adults, and their frequency increased with age. Risk factors that vary by age group may account for differences across age ranges.
The study population comprised 42 males (55%) and 34 females (45%), resulting in a male-to-female ratio of 1.23:1. This male predominance in gastrointestinal lesions aligns with findings reported in previous studies by Goel et al. (1.44:1), Kaur et al. (1.3:1), Margaret TJ et al., Shanmugasamy K et al., and Khandelia R et al. [10-14].
Most lesions occurred in the colon and rectum (n-29, 38.15%) followed by stomach (n-22, 28.94%). The lowest number of cases was seen in the ileum and ileocolic junction, with 2 cases each. A study by Rastogi G and Chawhan SM showed the large intestine and rectum to be the most common site of GI involvement, with 51 cases (51%), 22 (22%) cases in the stomach, and 3 (3%) cases in the ileum [9]. A study by Kaur et al. on non-malignant gastrointestinal lesions showed 110 cases (39.28%) in the colon and rectum [11]. Studies conducted by Sahu et al. and Kumawat et al. also identified the colorectum as the most frequently involved site [15, 16].
Among 76 cases, non-neoplastic cases were seen in 55 (72.3%) and neoplastic in 21 (27.63%). In the present study, non-neoplastic lesions demonstrated a broader spectrum of endoscopic findings than neoplastic lesions. Mucosal changes and ulceration or erosion was observed in 25% and 23.68% of non-neoplastic cases, respectively, reflecting the diverse inflammatory and reactive conditions affecting the gastrointestinal mucosa. In contrast, the predominant finding was neoplastic lesions that presented with growth, observed in 18.42% of cases (fig. 3). Interestingly, polyps were more frequently associated with non-neoplastic conditions (17.1%) than neoplastic ones (3.9%), suggesting that not all polypoid lesions should be assumed to have malignant potential. These findings underscore the importance of correlating endoscopic impressions with histopathological evaluation, as visual appearances alone may not reliably distinguish between benign and malignant pathologies.
In this study, ulcer-related lesions were the most frequent non-neoplastic findings, with ulcer and gastritis accounting for a significant proportion. Non-specific inflammation was common among inflammatory conditions, particularly in mucosal changes. In contrast, neoplastic cases predominantly presented as growths, with carcinoma being the most frequent diagnosis. Polypoid lesions were more commonly associated with non-neoplastic conditions, particularly polyps and Brunner gland hyperplasia. These trends, as visualized in fig. 3 and 4, emphasize the diagnostic diversity of non-neoplastic lesions compared to the more uniform presentation of neoplastic lesions.
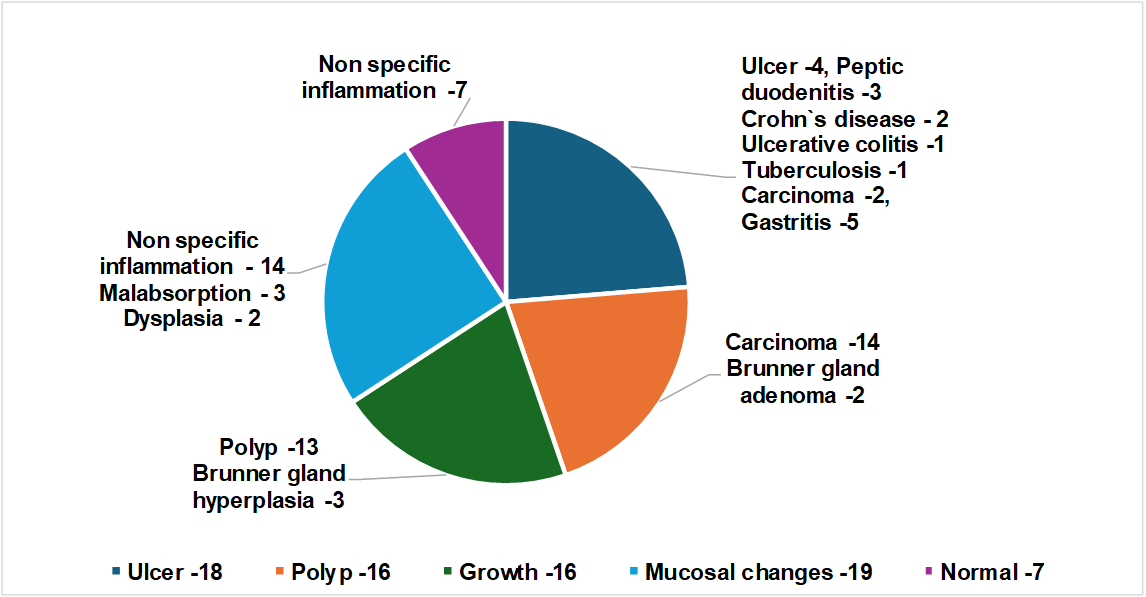
Fig. 3: Endoscopic and histopathological features of GI lesions
Correlation of endoscopic features with histopathology
The diagnostic performance of endoscopic features in detecting neoplastic lesions was evaluated using histopathology as the gold standard. To assess the diagnostic value of endoscopy in detecting neoplastic lesions, endoscopic findings were categorized as “suspicious” (growth and polyp) and “non-suspicious” (ulcer/erosion, mucosal changes, and normal). This classification revealed that endoscopy had a high sensitivity (80.9%) and negative predictive value (90%), indicating that it has effectively ruled out neoplastic lesions when suspicious features were absent. However, the positive predictive value was moderate (53%), suggesting that while suspicious findings often indicated neoplasia, they were not definitive without histopathological confirmation. The specificity was 72.7%, reflecting a fair ability to distinguish non-neoplastic from neoplastic lesions.
Statistical analysis using the Chi-square test demonstrated a significant association between endoscopic impressions and histopathological outcomes (χ² = 18.15, df = 1, p<0.0001). Furthermore, the diagnostic accuracy of endoscopy was 75%, meaning three out of four cases were correctly identified as neoplastic or non-neoplastic based on endoscopic appearance.
Cohen’s Kappa value of 0.67 indicates substantial agreement between endoscopic and histological diagnoses, reinforcing the reliability of endoscopy as a preliminary diagnostic tool. In comparison to the findings by Machiwal K et al., who reported a sensitivity of 96.25%, specificity of 68.67%, positive predictive value (PPV) of 74.76%, negative predictive value (NPV) of 95.0%, accuracy of 82.21%, and a kappa value of 0.57 (p<0.001), our study demonstrated a slightly lower sensitivity (80.9%) and accuracy (75%), but a higher specificity (72.7%) and kappa value (0.67), indicating better agreement between endoscopic and histopathological diagnoses [17]. While our PPV was lower (53%), the NPV remained high (90%), underscoring the reliability of endoscopy in ruling out neoplastic lesions.
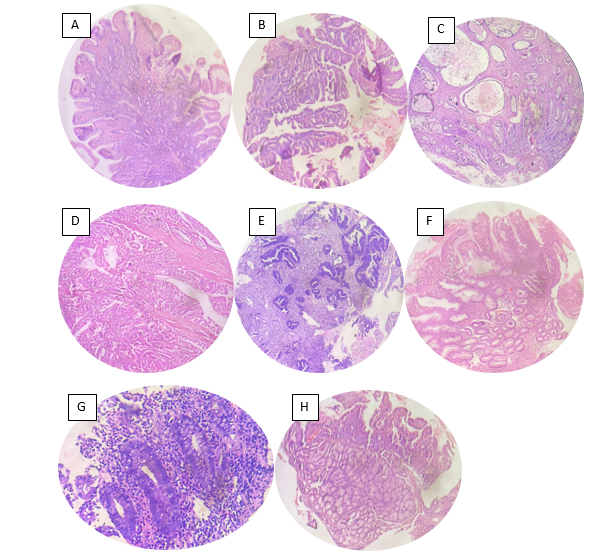
Fig. 4: A-Tubulovillous adenoma B-Colonic dysplasia C-Juvenile rectal polyp D, E-Adenocarcinoma F-Gastric Hyperplastic polyp stomach G-Crohn`s disease H-Brunner gland hyperplasia/adenoma (Hand E, 20X)
The correlation between endoscopic and histopathological diagnosis was 67% in this study, compared to 66.9% by Machiwal K. et al. An 88.8% correlation between the two diagnostic approaches was reported by Kazi et al., indicating a strong diagnostic agreement [18]. A study by Rauta et al. reported Cohen’s kappa score across all sites as 0.49(49%), indicating a moderate agreement between endoscopic and histopathologic diagnosis [5].
These findings underscore the value of endoscopy in clinical decision-making. However, the moderate positive predictive value reiterates that histopathological examination remains crucial for definitive diagnosis.
LIMITATIONS
One limitation of the present study is the relatively small sample size (n=76), which restricts the extrapolation of results to the broader patient population. Future studies with larger cohorts are needed to validate and generalize these findings.
CONCLUSION
This study emphasizes the value of endoscopy for detecting lesions in the gastrointestinal tract. Suspicious endoscopic findings like growth and polyps were strongly correlated with neoplastic lesions, while non-neoplastic lesions commonly presented as mucosal changes or ulceration. The high specificity and accuracy of endoscopy in diagnosing neoplastic lesions highlights its crucial role in clinical practice, especially in early cancer detection.
ACKNOWLEDGEMENTS
Nil
FUNDING
Nil
AUTHORS CONTRIBUTIONS
All authors have contributed equally
CONFLICTS OF INTEREST
Declared none
REFERENCES
Krishnappa R, Horakerappa M, Ali K, Gouri M. A study on histopathological spectrum of upper gastrointestinal tract endoscopic biopsies. Int J Med Res Health Sci. 2013;2(3):418-24. doi: 10.5958/j.2319-5886.2.3.073.
Pailoor K, Sarpangala MK, Naik RC. Histopathological diagnosis of gastric biopsies in correlation with endoscopy a study in a Tertiary Care Center. Adv Lab Med Int. 2013;3(2):22-31.
Isaacson P. Biopsy appearances easily mistaken for malignancy in gastrointestinal endoscopy. Histopathology. 1982 Jul;6(4):377-89. doi: 10.1111/j.1365-2559.1982.tb02735.x, PMID 7118078.
Deutsch JC. The optical biopsy of small gastric lesions. Gastrointest Endosc. 2014;79(1):64-5. doi: 10.1016/j.gie.2013.07.035, PMID 24342587.
Rauta S, Baisakh P, Sahoo AK, Panda DK, Baisakh MR, Dash SS. Correlation of endoscopic and histopathological diagnoses in upper gastrointestinal tract lesions: a cross-sectional study. Cureus. 2024 Sep 16;16(9):e69553. doi: 10.7759/cureus.69553, PMID 39421087, PMCID PMC11484197.
Saroha N, Ahamed MA. Histopathological study of neoplastic lesions of upper gastrointestinal tract endoscopic biopsies. Indian J Pathol Oncol. 2022;9(1):43-7. doi: 10.18231/j.ijpo.2022.010.
Rai NN, Agrawal MM. Histopathological spectrum of upper gastrointestinal lesions detected by endoscopy-guided biopsy-a single institute experience. IP Archives of Cytology and Histopathology Research. 2019;4(2):154-8. doi: 10.18231/j.achr.2019.029.
Sharma S, Kumari K, Sharad S, Shah G, Neelam. Histopathological spectrum of lesions in gastrointestinal endoscopic biopsy: a prospective study of 500 cases. Indian J Pathol Oncol. 2020;7(3):384-91. doi: 10.18231/j.ijpo.2020.077.
Rastogi G, Chawhan SM. Histopathology of endoscopic biopsies of gastrointestinal tract lesions with clinical correlation. Acta Med Int. 2023;10(2):79-90. doi: 10.4103/amit.amit_8_23.
Goel R, Bansal R, Jaiswal N. Clinico-histo-morphological spectrum of endoscopic biopsies of upper gastrointestinal tract. JK Sci J Med Educ Res. 2022;24(1):28-32.
Kaur M, Bhasin TS, Manjari M, Mannan R, Sharma S, Anand G. Correlation between histopathological and endoscopic findings of non-malignant gastrointestinal lesions: an experience of a Tertiary Care Teaching Hospital from Northern India. J Pathol Nep. 2018;8(1):1289-96. doi: 10.3126/jpn.v8i1.19456.
Margaret TJ, Lavanya M, Gerad RJ, Basha SK. Evaluating the spectrum of histomorphological patterns on endoscopic biopsy in patients with gastrointestinal tract disorders. Trop J Pathol Microbiol. 2020;6(1):12. doi: 10.17511/jopm.2020.i01.01.
Shanmugasamy K, Bhavani K, Anandraj Vaithy K, Narashiman R, Dhananjay SK. Clinical correlation of upper gastrointestinal endoscopic biopsies with histopathological findings and to study the histopathological profile of various neoplastic and non-neoplastic lesions. J Pharm Biomed Sci. 2016;6(4):220-4. doi: 10.20936/jpbms/160226.
Khandelia R, Saikia M. Histopathologic spectrum of upper gastrointestinal tract mucosal biopsies: a prospective study. IJMSCI. 2017;4(11):3314-6. doi: 10.18535/ijmsci/v4i11.11.
Sahu S, Suryakant WA, Jaiswal R. Endoscopic biopsies-a boon to diagnose gastrointestinal tract diseases. Int Arch Integr Med. 2019;6(12):47-56.
Kumawat DN, Shah DS, Goswami DH. A study of histopathological spectrum of gastrointestinal tract lesions in a Tertiary Care Centre. Int J Clin Diagn Pathol. 2021;4(2):9-12. doi: 10.33545/pathol.2021.v4.i2a.349.
Machiwal K, Menghani B, Kasliwal N, Sharma MP. Histopathological spectrum of lesions in gastrointestinal endoscopic biopsies in Jawahar Lal Nehru Medical College and associated group of Hospitals, Ajmer, Rajasthan. Int J Res Med Sci. 2022 Dec;10(12):2831-6. doi: 10.18203/2320-6012.ijrms20223084.
Kazi JI, Alam SM, Kazi AM, Anwar A, Shamsi Z. Correlation of endoscopic and histological diagnosis in upper gastrointestinal lesions. J Pak Med Assoc. 1990;40(12):281-3. PMID 2126566.