
Int J Curr Pharm Res, Vol 17, Issue 6, 133-137Original Article
PROPOLIS AND ITS ADVANCED FORMULATIONS: CURRENT PERSPECTIVES IN DENTAL APPLICATIONS
RIFAYA S., SIREEN ASHIKA A., MOHAMED ABSAL S., BHUVANESHWAR G., UBAIDULLA UTHUMANSHA*
Department of Pharmaceutics, Crescent School of Pharmacy, B. S. Abdur Rahman Crescent Institute of Science and Technology, GST Road, Vandalur, Chennai, Tamil Nadu, India
*Corresponding author: Ubaidulla Uthumansha; *Email: ubaidulla@crescent.education
Received: 12 Aug 2025, Revised and Accepted: 02 Oct 2025
ABSTRACT
Objective: To provide a detailed summary of advanced formulations of propolis for dental applications, focusing on strategies designed to enhance its therapeutic efficacy, solubility, stability, and overall clinical utility.
Methods: A comprehensive literature search was conducted using PubMed, Scopus, Web of Science, and Embase databases. Studies were included if they investigated propolis-based formulations relevant to dentistry, particularly those involving nanoparticles, nanoemulsions, mouth rinses, liposomes, or propolis incorporated into composites and sealants.
Results: Findings from the reviewed literature indicate that advanced delivery systems significantly improve the solubility, bioavailability, and biofilm penetration of propolis while prolonging its antimicrobial activity. Nanoparticles and nanoemulsions enhance propolis’s stability and therapeutic efficacy, whereas formulations such as mouth rinses, liposomes, and dental composites contribute to improved patient compliance, ease of administration, and usability. Collectively, these approaches support the role of propolis in dental caries prevention and overall oral health maintenance.
Conclusion: Advanced formulations of propolis successfully overcome limitations related to its natural form by enhancing stability, therapeutic performance, and patient-friendly delivery. Continued research should focus on clinical validation and the development of standardized propolis formulations for consistent and effective use in dental practice.
Keywords: Propolis, Dental applications, Advanced formulations, Dental caries, Drug delivery system
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijcpr.2025v17i6.8031 Journal homepage: https://innovareacademics.in/journals/index.php/ijcpr
INTRODUCTION
Dental caries is notable as a significant and persistent public health issue in dentistry. Customized brushing method, dietary changes and fluoride use are crucial in preventing carious lesions. Research indicates that incorporating “MISWAK” with proper technique alongside tooth brushing benefits both oral and systemic health. Similarly, various studies have examined the impact of propolis on the susceptibility of streptococcus mutans, caries formation, and glycosyl transferase activity in rats, revealing that propolis extract has cariostatic properties [1]. Additionally, consistent finding from author demonstrates that propolis extract reduces plaque buildup on teeth, thereby indirectly decreasing dental caries. Furthermore, Durate et al. found that the fatty acids in propolis offer a cariostatic effect by reducing microorganism tolerance to low pH and slowing acid production [2]. Recently, Nam et al. reported that Brazilian propolis exhibits significant antimicrobial effects against streptococcus mutans in the mouth by inhibiting enzyme activity and cell division [3]. He also concluded that propolis could serve as a natural alternative therapy for oral infection without reported side effects. A study by Cardoso et al. reported that the ethanolic extract of propolis does not inhibit the demineralization process in carries [4]. Dental diseases, including dental caries, periodontitis, and oral infections, remain a significant global health concern, affecting individuals across all age groups. Conventional therapeutic approaches, such as mechanical plaque removal and chemical antiseptics, often have limitations, including incomplete biofilm eradication, microbial resistance, and potential adverse effects. In recent years, natural products have garnered attention for their multifunctional bioactive properties and biocompatibility. Among these, propolis, a resinous substance produced by bees from plant exudates, has emerged as a promising candidate in oral healthcare due to its potent antimicrobial, anti-inflammatory, antioxidant, and immunomodulatory activities [5].
Despite its therapeutic potential, the clinical translation of propolis is often hindered by poor solubility, instability, and variability in composition. To overcome these challenges, advanced drug delivery systems such as chitosan-based nanoparticles, mucoadhesive hydrogels, nanoemulsions, and polymeric carriers have been developed to enhance the bioavailability, stability, and controlled release of propolis [6]. These formulations not only improve its efficacy against cariogenic bacteria like Streptococcus mutans but also offer targeted, sustained, and patient-friendly modes of application [7].
This review aims to provide a comprehensive overview of propolis and its advanced formulations in dental applications, summarizing current evidence on their mechanisms of action, therapeutic potential, and clinical relevance. By highlighting recent innovations in formulation strategies, this work seeks to inform future research and guide the development of effective propolis-based interventions for dentistry.
MATERIALS AND METHODS
The methodology for this review involved a systematic and comprehensive approach to evaluate current evidence on propolis and its advanced formulations in dental applications. A thorough literature search was conducted across multiple electronic databases, including PubMed/Medline, Scopus, Web of Science, Embase, and Cochrane Library, covering studies published up to September 2025. Keywords such as “propolis,” “dental applications,” “nanoparticles,” “mucoadhesive formulations,” “drug delivery systems,” and “biofilm inhibition” were used in combination with Boolean operators to refine the search. Studies were selected based on their investigation of propolis as a primary therapeutic agent in dentistry, particularly those exploring advanced delivery systems such as nanoparticles, hydrogels, or nanoemulsions, and reporting outcomes relevant to antimicrobial activity, caries prevention, or oral health enhancement. Excluded were review articles, conference abstracts, editorials, studies not related to dentistry, and publications lacking full text. Data extraction was performed independently by two reviewers, capturing details on formulation type, mode of action, experimental model, and key findings. The collected data were then qualitatively synthesized to summarize trends in propolis-based dental formulations, highlighting their advantages, limitations, and potential clinical applications.
Propolis as intracanal medicaments
Compared the effectiveness of three intracanal medicaments and propolis against E. faecalis and concluded that propolis as intracanal medicament inhibited growth and proliferation of E. faecalis and had right antibacterial efficacy. Awawdeh et al. compared propolis and calcium hydroxide as intracanal medicament and demonstrated that propolis was a fine intracanal medicament and reduced E. faecalis significantly [8]. De Rezende et al., assessed the antimicrobial action of two pastes containing propolis and calcium hydroxide vs polymicrobial cultures from root canals of 16 necrotic primary molars [9]. The agar well-diffusion technique was used to establish the antimicrobial activity of the following pastes: 11% ethanolic extract of propolis+calcium hydroxide; and 11.0% extract of propolis without ethanol+calcium hydroxide. Results indicated that anti-microbial activity of the latter paste was superior than the former paste 1 (P=0.053). Overall, however, both pastes exhibited high antimicrobial activity. They opined that combination of propolis and calcium hydroxide is efficient to control dental infections.
Propolis as a treatment for dentin hypersensitivity
Mahmoud and associates have evaluated the efficacy of propolis on dentin hypersensitivity. Using electron microscopy, they found propolis occluded the dentinal tubules. The clinical efficacy of casein phosphor peptide amorphous calcium phosphate fluoride, sodium fluoride, propolis and distilled water after 8 d, 60 d, and 3 mo of use. The authors noted that propolis was the most effective material for managing dentin hypersensitivity. While all materials were superior than distilled water, they differed in the time of effect over the three months [10].
Propolis as a pulp capping material
The treatment outcomes were equivalent to those of mineral trioxide aggregate and calcium hydroxide. The properties of propolis being resinous and adhesive is effective as it seals dentinal tubules and possesses anti-inflammatory properties, reducing pulpal inflammation. Furthermore, Sabir et al. investigated the dental pulp responses of rats treated with direct pulp capping using propolis. Nine rats were divided into three groups. Class 1 cavities were prepared on the occlusal surface of the maxillary right first molars. The dental pulp was exposed, and either the zinc oxide-based filler, propolis flavonoids, or propolis non-flavonoids were placed in the cavities. The study found that dental pulp capping with propolis flavonoids in rats delayed pulpal inflammation and promoted dentin regeneration [11].
Propolis for treatment of periodontitis
Murray et al. studied the effect of a mouth rinse with propolis, a chlorhexidine rinse and a placebo on the formation of microbial plaques [12]. Chlorhexidine was much more effective than either of the two other rinses, and prevented plaque formation altogether. Propolis mouth rinse demonstrated some benefit over that of the negative control and the difference was not statistically significant. The difference in the results of these two studies may be attributable to the difference in methodologies. Koo et al. looked at the efficacy of a mouth rinse containing RS-SNB propolis on dental plaque [13].
Propolis versus other mouthwash
Ozan et al. studied the effectiveness of propolis solutions at different concentrations (1, 2.5, 5 and10%) and compared it to a control mouthwash containing 0.2% chlorhexidine [14]. They conducted experiments to evaluate efficacy against oral organisms and effects on human gingival fibroblasts for each mouthwash. Chlorhexidine was more effective against microorganisms but was also more cytotoxic to human gingival fibroblasts. Propolis can also help maintain oral health and even reduce children caries due to its antibiotic and anti-plaque properties. A simple propolis mouthwash can be made by mixing 10–50 drops of propolis to one glass of warm water. Propolis mouth rinse can sometimes be swallowed with potential additional benefit compared to conventional mouthwashes.
Propolis in caries prevention
Hayacibara et al. investigated propolis effects on the viability of Streptococcus mutans, glucosyltransferase activity and the extent of caries in rats [15]. They concluded that propolis was an effective caries prevention agent, since it inhibited the activity of glucosyltransferase enzyme. The same conclusion was reached by Ikeno et al. [16] Koo et al. also studied propolis constituents and their effect on the glucosyltransferase enzyme activity, caries extent in general, and found one specific propolis constituent-apigenin-was strong in inhibiting glucosyltransferase activity [17].
Propolis as intracanal irrigant
Qathami and Al-Madi compared the antimicrobial efficacy of intracanal irrigation by propolis, sodium hypochlorite and salt [18]. Microbial sample was collected on immediate canal opening, access cavity preparation and root canal preparation and irrigation. They checked the influence of propolis on colony forming unit count. The findings from the current study proved that the antimicrobial potential of propolis was as effective as that of sodium hypochlorite. Kandaswamy et al. separated 180 extracted teeth inoculated with Enterococcus faecalis for 21 d into six groups based on the intracanal irrigant solution to be utilized (Saline, propolis, MCJ, 2% povidone iodine, 2% chlorhexidine gel and calcium hydroxide) [19]. The dentinal tubule colonies that were viable at 200 and 400 µ depths were counted one, three and five days later. The findings were in such a way that chlorhexidine gluconate (100%) was more potent in its antimicrobial activity compared to 2% povidone iodine (87%), propolis (71%), MCJ (69%) and calcium hydroxide (55%). No difference was observed in the activity of propolis and MCJ at 200 or 400 µm depths. The findings revealed that propolis and MCI suppressed E. faecalis growth in dentin of extracted teeth.
Propolis used as a cavity disinfectant
Effective caries prognosis is closely linked to the removal of infected dentin (fig. 1). With a better understanding of the caries process, there have been significant advancement in managing carious lesions. Cavity disinfection serves as an additional method to lower or eliminate bacterial presence in the remaining dentin after cavity preparation. Propolis along with other disinfectants like APH (acidulated phosphate fluoride) gels, diode lasers, and 2% chlorhexidine, was tested against Streptococcus mutans showing a notable reduction in bacterial count across all groups. In comparison, APF gels were the least effective, whereas Brazilian propolis and diode lasers showed similar levels of effectiveness to the 2% chlorhexidine control group. Research by Prabhakar et al., along with other studies, suggested that both aloe vera and propolis have the potential to serve as cavity disinfectants after minimally invasive hand excavation [20].
Advanced propolis-based formulations in dentistry
Advanced propolis-based formulations in dentistry utilize modern drug delivery systems to overcome the limitations of raw propolis, such as poor solubility and rapid degradation. Nanoparticles, such as chitosan-propolis NPs, enhance solubility, bioavailability, and controlled release while penetrating dental biofilms [21-25]. Nanoemulsions improve diffusion into plaque and provide stable, highly antimicrobial formulations. Mouthrinses and varnishes offer an easy-to-use preventive approach with direct antimicrobial and fluoride-like protective effects. Liposomes protect the active compounds, enable controlled release, and improve biofilm penetration [26-28]. Dental composites and sealants provide continuous antimicrobial action, prevent secondary caries, and combine restorative and therapeutic benefits. Collectively, these advanced formulations significantly enhance the efficacy, stability, and clinical applicability of propolis in caries prevention and overall oral healthcare.
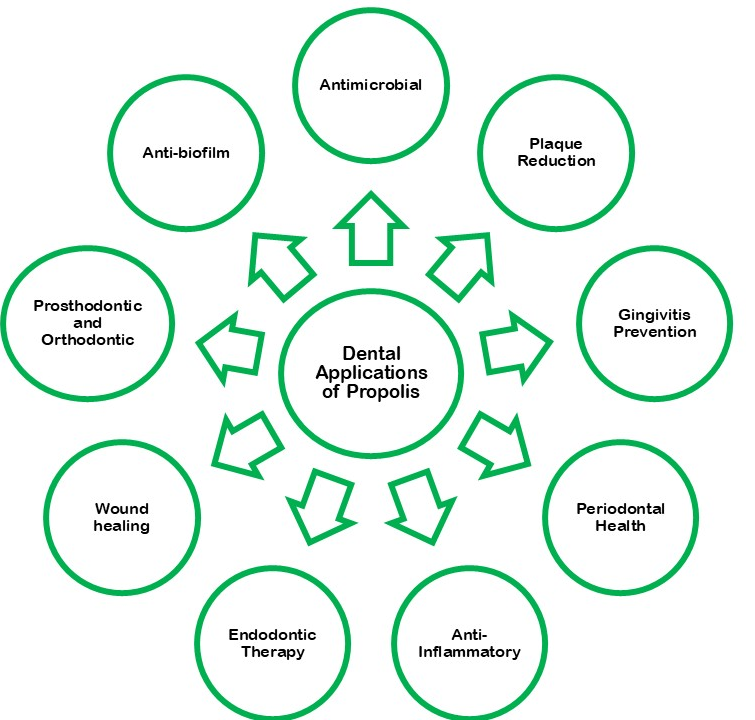
Fig. 1: Schematic representation of dental applications of propolis

Fig. 2: Propolis used delivery platforms to improve its therapeutic effectiveness in dentistry
Propolis has been formulated into diverse delivery platforms to improve its therapeutic effectiveness in oral disease and caries management (fig. 2). Nanoparticles, particularly those based on chitosan and other polymers, provide sustained release, enhance bioavailability, and penetrate biofilms, thereby significantly reducing plaque formation and caries lesions. Nanoemulsions, usually oil-in-water systems, improve solubility and diffusion of propolis, resulting in enhanced antimicrobial activity and effective inhibition of Streptococcus mutans. Similarly, mouthrinses and varnishes containing propolis offer simple, preventive, and patient-friendly applications with fluoride-like protective action, contributing to reduced salivary S. mutans counts and plaque scores. Advanced carriers such as liposomes protect the bioactive components from degradation, enable controlled release, and enhance antibacterial as well as anti-inflammatory effects (table 1). In restorative dentistry, propolis-infused composites and sealants act dually by restoring tooth structure and releasing antimicrobials continuously, thereby preventing secondary caries [29, 30]. Biopolymeric hydrogels, composed of chitosan or alginate, allow controlled release through swelling and diffusion, prolonging antimicrobial action while adhering effectively to oral mucosa. Likewise, electrospun fibers of polycaprolactone provide high surface area and controlled degradation, supporting localized antimicrobial delivery within cavities. Mucoadhesive films and patches extend contact time in the oral cavity, improving compliance and enabling direct diffusion into saliva and mucosa. Microspheres, such as PLGA-based systems, release propolis through polymer erosion, offering longer stability and sustained antimicrobial activity compared to free propolis. Finally, toothpastes and mouthrinses incorporated with propolis provide a convenient, patient-friendly approach for daily oral care, reducing bacterial load and inflammation. Collectively, these delivery systems demonstrate the versatility of propolis in preventive and therapeutic strategies against dental caries and oral diseases [31].
Table 1: Propolis-incorporated delivery systems: formulations and clinical relevance in caries control
| Delivery system | Formulation/Material used | Advantages in caries/Oral disease management |
| Nanoparticles | Chitosan–propolis NPs, polymeric nanoparticles | Enhanced bioavailability, biofilm reduction, biocompatibility |
| Nanoemulsion | Oil-in-water nanoemulsion with propolis extract | Increased antimicrobial activity, stable formulation |
| Mouthrinse/Varnishes | Propolis extract in mouthrinse or varnish | Easy application, preventive approach |
| Liposomes | Phospholipid-based liposomes encapsulating propolis | Enhanced stability, antibacterial and anti-inflammatory effects |
| Dental Composites/Sealants | Resin composites or sealants infused with propolis | Prevents secondary caries, dual restorative–therapeutic role |
| Hydrogels | Chitosan–propolis or alginate–propolis hydrogel | Prolonged antibacterial effect, bioadhesive to oral mucosa |
| Electrospun Fibres | Polycaprolactone/propolis composite fibers | High surface area, flexibility, local delivery to cavities |
| Films/Patches | Mucoadhesive oral films containing propolis | Prolonged contact time, improved patient compliance |
CONCLUSION
This current review focused on pharmacological properties of propolis s pharmacological application propolis has been used dental carries treatment. Since few decades in this paper currently focused on various method. We have full review on applications of propolis especially dental carries management. The propolis has been treatment for dental disease but it has limitation like low water soluble and poor bioavailability nanoparticles has been mainly we use to overcome the limitation of propolis. The review covers the current advanced propolis formulations explore therapeutic improvement of the propolis. This review paper enlists in the propolis and its formulation as well as therapeutic usages in dentistry.
FUNDING
Nil
AUTHORS CONTRIBUTIONS
The authors are thankful to the Management of B. S. Abdur Rahman Crescent Institute of Science and Technology for their support and encouragement in successfully completing this work.
CONFLICT OF INTERESTS
Declared none
REFERENCES
Duane B, Yap T, Neelakantan P, Anthonappa R, Bescos R, McGrath C. Mouthwashes: alternatives and future directions. Int Dent J. 2023 Nov;73 Suppl 2:S89-97. doi: 10.1016/j.identj.2023.08.011, PMID 37867066.
Duarte S, Rosalen PL, Hayacibara MF, Cury JA, Bowen WH, Marquis RE. The influence of a novel propolis on mutans Streptococci biofilms and caries development in rats. Arch Oral Biol. 2006;51(1):15-22. doi: 10.1016/j.archoralbio.2005.06.002, PMID 16054589.
Nam SH. Antimicrobial activity of propolis on different oral bacteria. Indian J Sci Technol. 2015;8(1):1-4. doi: 10.17485/ijst/2016/v9i15/89174.
Cardoso JG, Iorio NL, Rodrigues LF, Couri ML, Farah A, Maia LC. Influence of a Brazilian wild green propolis on the enamel mineral loss and Streptococcus mutans count in dental biofilm. Arch Oral Biol. 2016;65:77-81. doi: 10.1016/j.archoralbio.2016.02.001, PMID 26871983.
Khurshid Z, Naseem M, Zafar MS, Najeeb S, Zohaib S. Propolis: a natural biomaterial for dental and oral healthcare. J Dent Res Dent Clin Dent Prospects. 2017;11(4):265-74. doi: 10.15171/joddd.2017.046, PMID 29354255.
Coutinho A. Honeybee propolis extract in periodontal treatment: a clinical and microbiological study of propolis in periodontal treatment. Indian J Dent Res. 2012;23(2):294. doi: 10.4103/0970-9290.100449, PMID 22945731.
Afrasiabi S, Pourhajibagher M, Chiniforush N, Bahador A. Propolis nanoparticle enhances the potency of antimicrobial photodynamic therapy against Streptococcus mutans in a synergistic manner. Sci Rep. 2020 Sep 23;10(1):15560. doi: 10.1038/s41598-020-72119-y, PMID 32968097.
Awawdeh L, Al Beitawi M, Hammad M. Effectiveness of propolis and calcium hydroxide as a short-term intracanal medicament against Enterococcus faecalis: a laboratory study. Aust Endod J. 2009 Aug;35(2):52-8. doi: 10.1111/j.1747-4477.2008.00125.x, PMID 19703075.
De Rezende GP, Da Costa LR, Pimenta FC, Baroni DA. In vitro antimicrobial activity of endodontic pastes with propolis extracts and calcium hydroxide: a preliminary study. Braz Dent J. 2008;19(4):301-5. doi: 10.1590/s0103-64402008000400003, PMID 19180318.
Mahmoud AS, Almas K, Dahlan AA. The effect of propolis on dentinal hypersensitivity and level of satisfaction among patients from a University Hospital Riyadh, Saudi Arabia. Indian J Dent Res. 1999;10(4):130-7. PMID 10865396.
Sabir A, Tabbu CR, Agustiono P, Sosroseno W. Histological analysis of rat dental pulp tissue capped with propolis. J Oral Sci. 2005;47(3):135-8. doi: 10.2334/josnusd.47.135, PMID 16313091.
Murray MC, Worthington HV, Blinkhorn AS. A study to investigate the effect of a propolis-containing mouthrinse on the inhibition of de novo plaque formation. J Clin Periodontol. 1997;24(11):796-8. doi: 10.1111/j.1600-051X.1997.tb01191.x, PMID 9402499.
Koo H, Vacca Smith AM, Bowen WH, Rosalen PL, Cury JA, Park YK. Effects of Apis mellifera propolis on the activities of streptococcal glucosyltransferases in solution and adsorbed onto saliva-coated hydroxyapatite. Caries Res. 2000;34(5):418-26. doi: 10.1159/000016617, PMID 11014909.
Ozan F, Sumer Z, Polat ZA, Er K, Ozan U, Deger O. Effect of mouthrinse containing propolis on oral microorganisms and human gingival fibroblasts. Eur J Dent. 2007 Oct;1(4):195-201. doi: 10.1055/s-0039-1698339, PMID 19212467, PMCID PMC2609911.
Hayacibara MF, Koo H, Rosalen PL, Duarte S, Franco EM, Bowen WH. In vitro and in vivo effects of isolated fractions of Brazilian propolis on caries development. J Ethnopharmacol. 2005 Oct 3;101(1-3):110-5. doi: 10.1016/j.jep.2005.04.001, PMID 15913934.
Ikeno K, Ikeno T, Miyazawa C. Effects of propolis on dental caries in rats. Caries Res. 1991;25(5):347-51. doi: 10.1159/000261390, PMID 1836157.
Koo HJ, Lee KR, Kim HS, Lee BM. Detoxification effects of aloe polysaccharide and propolis on the urinary excretion of metabolites in smokers. Food Chem Toxicol. 2019 Aug;130:99-108. doi: 10.1016/j.fct.2019.05.029, PMID 31112706.
Al Qathami H, Al Madi E. Comparison of sodium hypochlorite propolis and saline as root canal irrigants: a pilot study. Saud Dent J. 2003;15(2):100-3.
Kandaswamy D, Venkateshbabu N. Root canal irrigants. J Conserv Dent. 2010;13(4):256-64. doi: 10.4103/0972-0707.73378, PMID 21217955.
Prabhakar AR, Karuna YM, Yavagal C, Deepak BM. Cavity disinfection in minimally invasive dentistry: comparative evaluation of Aloe vera and propolis: a randomized clinical trial. Contemp Clin Dent. 2015 Mar;6 Suppl 1:S24-31. doi: 10.4103/0976-237X.152933, PMID 25821369, PMCID PMC4374313.
Sandhiya V, Ubaidulla U. Herbal nanomedicines and cellular uptake mechanism. In: Thomas S, Oyedeji AO, Oluwafemi OS, Rose Jaquilin PJ, editors. Nanotechnology in herbal medicine. Woodhead Publishing Series in Biomaterials; Elsevier; 2023. p. 63‑99. doi: 10.1016/B978‑0‑323‑99527‑6.00011‑2.
Sandhiya V, Elumalai S, Dhunmati K, Nalini CN, Mani G, Balakrishnan S. Chapter: toxicity of nanoparticles, recent advances and new perspectives. In: Muzibur Rahman M, Uddin J, Mohamed Asiri A, Rezaur Rahman M, editors. Toxicity of Nanoparticles Recent Advances and New Perspectives. London (UK): IntechOpen; 2024. doi: 10.5772/intechopen.112074.
Uthumansha U, Vengateswaran HT, Habeeb M, Navabshan I, Sandhiya V, Priyanka Sinha Y. Exploring nature’s pharmacy: breakthroughs in herbal drug development and technology. In: Futuristic Trends in Pharmacy & Nursing Volume 3, Book 6; 2024. p. 282‑97. Available from: https://iipseries.org/assets/docupload/rsl202438AEA13B4B7C615.pdf. [Last accessed on 05 Nov 2025].
Ubaidulla U, Senthil Kumar B, Ahmad FJ, Khar RK. Studies on suspension of nimesulide solid dispersion: development, characterization and in vivo evaluation. Indian J Pharm Sci. 2005;67(4):422-6.
Prabahar K, Uthumansha U, Elsherbiny N, Qushawy M. Enhanced skin permeation and controlled release of β-sitosterol using cubosomes encrusted with dissolving microneedles for the management of alopecia. Pharmaceuticals (Basel). 2023;16(4):563. doi: 10.3390/ph16040563, PMID 37111320.
Sandhiya V, Ubaidulla U. Enhancing cellular uptake and membrane permeability of gallic acid for breast cancer therapy via folate-tagged pegylated iron oxide nanoparticles has theronastic agent. Bull Natl Res Cent. 2022;46(1):234. doi: 10.1186/s42269-022-00909-7.
Charumathy A, Ubaidulla U, Sinha P, Rathnam G. Recent update on liposome-based drug delivery system. Int J Curr Pharm Res. 2022 May;14(3):22-7. doi: 10.22159/ijcpr.2022v14i3.1991.
Rama B, Sandhiya V, Swetha M, Rathnam G, Ubaidulla U. Pulsatile drug delivery: a comprehensive review. IJPDT. 2015;5(2):125-30.
Mohan J, Deepa L, Ubaidulla U, Ganesh N. In vitro antioxidant activity of hydro alcoholic extract of Gynocardia odorata roxb. Leaf. Int J Res Pharm Nano Sci. 2013;2(3):351-7.
Loganathan V, Sreekanth N, Kumar BS, Ubaidulla U, Reddy MVS, Manimaran S. Antibacterial activity of Vitex negundo Linn. Hamdard Med. 2004;47(3):29-32.
Hamze F, Amiri M, Islami ZS, Shamspur T, Razavi R, Khazaeli P. Synthesis and evaluation of antibacterial and antioxidant effects of propolis nanoparticles and cinnamon nanostructures in preventive dentistry: experimental and theoretical approaches. Phytochem Anal. 2024 Jul 7. doi: 10.1002/pca.3405, PMID 38973088.