
Int J Pharm Pharm Sci, Vol 17, Issue 9, 8-14Review Article
MINI TABLETS IN MODERN PHARMACEUTICS: A COMPREHENSIVE REVIEW OF FORMULATION, EVALUATION, AND CLINICAL APPLICATIONS
BISHAL SARKAR*
Department of Pharmaceutics, Mata Gujri College of Pharmacy, Kishanganj, Bihar-855107, India
*Corresponding author: Bishal Sarkar; *Email: grpbishal@gmail.com
Received: 25 May 2025, Revised and Accepted: 28 Jun 2025
ABSTRACT
The purpose of this review is to analyze the new role of mini tablet technology in pharmaceutical sciences by assessing its formulation approach, manufacturing process, quality evaluation parameters, and therapeutic use, especially in improving patient compliance and maximizing drug delivery. A systematic review of literature was performed using peer-reviewed journals, patents, and regulatory guidelines related to mini tablet formulation and testing. Manufacturing processes like direct compression, wet granulation, dry granulation, and melt-extrusion were critically appraised. Important test parameters like weight variation, hardness, friability, disintegration, dissolution profiles, and drug-excipient compatibility studies were evaluated. Mini tablets, often smaller than 3 mm in diameter, present benefits like enhanced accuracy of dosing, swallowability, and the possibility of multi-unit dosage forms. Mini tablets can be formulated for immediate, delayed, or prolonged drug release. Pediatric, geriatric, and dysphagic patients are especially well-served by such forms. Specialized systems such as enteric-coated and bioadhesive mini tablets have also indicated favorable results in controlled and targeted drug delivery. Multiple reports of successful therapeutic uses in cardiovascular, neurological, and gastrointestinal diseases have been documented in various studies. Mini tablet technology offers a flexible and patient-friendly option to traditional dosage forms. Its flexibility, ease of manufacture, and advantageous therapeutic profiles favor its wider application in contemporary pharmaceutics. Additional industrial uptake and research are necessary to fully maximize its potential in personalized and precision drug delivery systems.
Keywords: Mini tablets, Solid oral dosage forms, Modified drug release, Pharmaceutical evaluation, Pediatric and geriatric formulations
© 2025 The Authors. Published by Innovare Academic Sciences Pvt Ltd. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
DOI: https://dx.doi.org/10.22159/ijpps.2025v17i9.55477 Journal homepage: https://innovareacademics.in/journals/index.php/ijpps
INTRODUCTION
Oral solid dosage forms continue to be the most common drug delivery systems by virtue of their convenience, ease of use, patient acceptability, and cost. Among them, tablets are the largest market share-holders by virtue of their precise dosing, long shelf life, and large-scale production. But traditional tablets are plagued with limitations such as delayed onset of action, swallowing, particularly in pediatric and geriatric cases and lack of dosing flexibility. These constraints have evoked interest in the creation of new delivery systems like fast-disintegrating tablets (FDTs) and mini tablets, both with a view to improving patient-oriented therapy [1]. Mini tablets are solid multiple-unit dosage forms with a diameter usually less than or equal to 3 mm, though some sources raise the size to 6 mm based on use [2]. They have the advantage of being smaller compared to traditional tablets, particularly in patients with difficulty swallowing. Mini tablets differ from single-unit dosage forms as they can pass easily through the pylorus and reduce gastric retention time variability, hence enhancing the predictability of absorption. Such a feature is particularly beneficial for compounds with a limited window of absorption or are sensitive to gastric emptying rate [2]. The multi-unit structure of mini tablets allows for tailor-made drug release patterns such as immediate, sustained, pulsatile, and gastro-retentive release. Mini tablets can be coated or uncovered individually based on the therapeutic requirement, and hence, pharmacokinetics can be customized. This renders them suitable for use in personalized medicine, polypharmacy, and modified release systems, particularly when more than one active or release pattern is needed in a single dosage form [3]. For pediatric and geriatric practice, swallowability and flexibility of dose are critical. Mini tablets can be taken straight, inserted in sachets, or filled in capsules, and even blended with soft food or liquids, rendering them better than syrups or standard tablets as far as dosing accuracy and stability are concerned [4]. In addition, they reduce the hazard of dose dumping a risk associated with chewed or crushed tablets by releasing controlled and separate depots of the drug in the gastrointestinal tract. They decrease local gastrointestinal irritation if designed for drugs having mucosal sensitivity [5]. Mini tablet manufacturing usually uses multi-tip tooling on standard rotary tablet presses, with tight control of compaction and granule flow necessary because of the low die volume. Although very similar to normal tablet production, difficulties include meeting uniform die fill, not damaging the tooling, and batch uniformity [6]. The development of mini tablets aligns with the goals of modern pharmaceutics: improving bioavailability, enhancing patient compliance, enabling dose titration, and facilitating combination therapy in a compact, scalable, and flexible platform [7].
Literature search strategy
A thorough literature search was done through electronic databases such as PubMed, Scopus, ScienceDirect, and Google Scholar to compile this review. Boolean operators (AND/OR) inter fused search terms such as "mini tablets," "multi-unit dosage forms," "drug delivery systems," "sustained release," and "pediatric formulations" were searched. Articles between the years 2010 and 2025 were included. Only peer-reviewed journal articles, reviews, and regulatory reports published in the English language were included. Further references were obtained through manual citation search for completeness and relevance.
Constituents and release profile of mini-tablets
Mini-tablets provide a flexible vehicle for the placement of more than one drug substance, which is useful in the formulation of fixed-dose combinations and site-specific delivery systems. More than one mini-tablet can be packed into a capsule, each designed to have a unique release profile—like immediate release (IR), delayed release (DR), or controlled release (CR)—to release drugs in a particular location and over different durations [8]. This strategy enables the concomitant administration of incompatible drugs, enhancing therapeutic efficiency and promoting the treatment of comorbid diseases in one dosage form. Release kinetics of mini-tablets are controlled by their formulation ingredients and coating technologies. Their high surface area-to-volume ratio makes mini-tablets have higher dissolution and absorption rates than traditional tablets. In addition, hydrophilic matrix-forming polymers like Hydroxypropyl Methylcellulose (HPMC K100M) mini-tablets can release the drug over a longer period. Changing the amount of Hydroxypropyl Methylcellulose adjusts the density and rate of hydration of the matrix, giving complete control of drug diffusion [9]. Uniform film coatings of polymers can also adjust the release pattern, providing delayed or targeted drug release. Further, a mini-tablet composition can contain subpopulations of tablets with different release profiles (e. g., some for immediate release and others for extended release), yielding biphasic or pulsatile pharmacokinetics. This modularity renders mini-tablets prime candidates for chronotherapy, colon-targeted treatment, and multi-phase release.
Table 1: Difference between conventional tablets and mini tablets
| Properties | Conventional tablets | Mini Tablets | References |
| Size | >6 mm | ≤3 mm (up to 6 mm in some cases) | [1–3] |
| Swallowability | Difficult for pediatric/geriatric populations | Excellent for all age groups | [2,4] |
| Dose flexibility | Fixed dose | High—can combine units for adjustable dosing | [2,4] |
| Absorption predictability | Affected by gastric emptying | Improved due to easier pyloric passage | [3,5] |
| Drug release profiles | Limited (mainly immediate/sustained) | Versatile (immediate, pulsatile, delayed) | [4–6] |
| Personalization | Challenging | Facilitates personalized medicine | [5–6] |
| Risk of dose dumping | High if chewed or broken | Low—each unit functions independently | [6–7] |
| Manufacturing challenges | Standard tooling | Requires precise flow, modified tooling | [1,7] |
Benefits of mini-tablets
Mini-tablets have several pharmaceutical and technological benefits compared to conventional tablets, pellets, and multi-particulate systems. Mini-tablets are simple and reproducible to produce short runs with regular tablet presses and multi-tip tooling to facilitate high-throughput production [10]. Mini-tablets can have high drug loading and support a wide range of customizable drug release profiles [10]. The small tablets are of uniform shape, smooth surface, and equal size, which offer better flow properties and allow uniform coating to be deposited [11]. The individual mini-tablet is an individual drug depot which minimizes the risk of dose dumping and delivers drugs in a safer way [11]. Better gastrointestinal (GI) distribution of the small units reduces local drug concentrations and prevents mucosal irritation. This preparation also provides greater reduction in inter-and intra-subject variability and therefore more uniform pharmacokinetic profiles [12]. Mini-tablets are easier to manufacture than pellets because they do not involve sophisticated operations such as spheronization, extrusion, or fluid-bed granulation [13]. Due to their low porosity and high homogeneity of the surface, they provide better mechanical strength and improved coating performance. Besides, the solvent-free production capability facilitates the avoidance of stability problems related to solvent-based processing [9, 10]. Reproducibility is also increased by consistency of geometry and weight, whereas batch-to-batch consistency renders the mini-tablets stable and effective drug dosage form for current drug delivery systems.
Table 2: Comparative benefits of mini-tablets vs. pellets
| Properties | Mini-tablets | Pellets | References |
| Manufacturing complexity | Simple tableting with multi-tip tooling | Requires extrusion, spheronization, or fluid-bed granulation | [10–12] |
| Solvent use | Can be manufactured without solvents | Often requires solvent-based processes | [10–12] |
| Coating efficiency | High due to smooth surface, uniform size, low porosity | Difficult due to high porosity and irregular shape | [13] |
| Mechanical strength | High | Variable | [13] |
| Inter-/intra-subject variability | Low | Moderate to high | [12–14] |
| Dose flexibility | High-combination of release profiles in one capsule | Moderate | [11–14] |
| Scale-up potential | Easy and reproducible | Challenging | [10,12] |
| Application in pediatrics | Highly suitable (small size, easy swallowability) | Less ideal (hard to dose-split or control) | [13–15] |
Opportunities for the development of mini-tablet dosage forms
Mini-tablet technology provides flexible formulation approaches adapted to diverse therapeutic objectives and patient requirements. These approaches comprise compressed mini-tablets, coated encapsulated mini-tablets, and biphasic drug delivery systems, each designed for particular pharmacokinetic profiles and drug release patterns.
Compressed mini-tablets
Mini-tablets can be compressed directly into tablet shapes to avoid the expense and complexity of using hard gelatin capsules, lowering costs and manufacturing complexity. Their regular diameter, smooth appearance, low porosity, and high mechanical resistance account for better compressibility and content uniformity than granules or pellets [16]. By controlling the nature of the outside polymer matrix (e. g., hydrophobic or hydrophilic), and the amount of mini-tablets per compressed unit, specific release profiles can be optimized. This is especially useful for biphasic drug delivery, where one phase can provide immediate release to accommodate rapid action, and the other delivers sustained release to provide lasting therapeutic action [13–15].
Encapsulated coated mini-tablets
Coated mini-tablets have also been encapsulated in hard gelatin or Hydroxypropyl Methylcellulose capsules for the preparation of modular, multi-unit drug delivery systems. Mini-tablets may have some release profiles, such as rapid-release (RMTs), sustained-release (SMTs), pulsatile, or delayed-onset sustained-release mini-tablets (DSMTs), which are very compatible with multifunctional and chronotherapeutic applications [17]. Such a system allows for the co-delivery of drugs with different physicochemical properties in addition to fine adjustment of onset and duration of action. The entrapment of mini-tablets also reduces the risk of dose dumping, enhances gastrointestinal tolerability, and enhances overall therapeutic compliance. Spatial and temporal independence of individual units allows for site-specific and time-dependent drug delivery. Through the combination of miniature tablets with varying pharmacological composition, strength of dose, or release rate in one capsule, the system makes individualized and patient-directed therapy possible [18].
Biphasic drug delivery systems based on compressed mini-tablets
Biphasic drug delivery systems are designed to release a drug at two different rates or time periods, either fast/slow or slow/fast. In a usual fast/slow system, an early burst release is exhibited as rapid onset followed by sustained-release to ensure plasma drug concentration in the therapeutic window [19]. Such a system is especially useful for: NSAIDs, Antihistamines, Antihypertensives, Antiallergics. Formulations such as traditional sustained-release tablets tend to withhold therapeutic levels, and immediate-release granules do not have extended efficacy. Biphasic mini-tablet systems overcome this issue by incorporating a portion of the dose in the matrix fill (quick release) and another in coated mini-tablets (extended release) [20]. Not only does this provide consistent plasma profiles, but also minimizes the frequency of dosing and enhances patient compliance.
Table 3: Various approaches to mini-tablet formulations and their applications
| Type | Description | Applications | References |
| Compressed mini-tablets | Mini-tablets compressed directly into tablet form without capsule shell | Cost-effective, suitable for fast/slow biphasic release | [15, 16] |
| Encapsulated coated mini-tablets | Multiple coated mini-tablets encapsulated into Hydroxypropyl Methylcellulose/gelatin capsules | Modular dosing, multi-phase and multi-drug delivery | [16, 17] |
| Biphasic mini-tablet systems | Combines immediate and sustained release mini-tablets in one unit | Chronotherapy, rapid onset+prolonged action (e. g., NSAIDs) | [17, 18] |
| Rapid-release mini-tablets (RMTs) | Uncoated or disintegrant-based mini-tablets for fast action | Emergency relief, breakthrough symptoms | [18] |
| Sustained-release mini-tablets (SMTs) | Coated with hydrophobic/matrix polymers for controlled drug release | Chronic conditions requiring steady-state plasma concentrations | [18, 19] |
| Pulsatile mini-tablets (PMTs) | Engineered with time-dependent coatings for circadian rhythm targeting | Hormonal therapy, asthma, hypertension (nighttime dosing) | [19, 20] |
Types of mini tablets
Mini tablets are an adaptable solid dosage form that can be tailored according to drug characteristics, therapeutic objectives, and patient-specific requirements like age, ability to swallow, and ailment status. Mini tablets can be categorized into the following broad types depending on the action site, release pattern, target population, and formulation technology.
Pediatric mini tablets
Classic pediatric formulations such as syrups, tablets, and capsules have some shortcomings. Syrups can be affected by stability problems (chemical, microbiological), bad taste, and inadequate dose control. Tablets, because of their size, can pose swallowing problems and usually need breaking, which can lead to dosage inaccuracy and drug performance issues. Mini tablets, because of their compact size (usually 2–3 mm), accurate dosing, and swallowability, provide a perfect alternative for pediatrics. Children have been proved to accept mini tablets more than traditional solid or liquid dosage forms by studies. The formulations can also be developed for immediate, sustained, or delayed release to enhance the therapeutic effects [22].
Oral disintegrating mini tablets (ODMTs)
Oral Disintegrating Mini Tablets are designed to quickly disintegrate in the mouth (within 1–3 min), without needing water or chewing. Their good mouthfeel, taste-masking, and ease of administration make them suitable for pediatric, geriatric, and dysphagic patients. The breakdown leads to the creation of a soft paste or suspension and easy swallowing. Because the drug is dissolved close to the taste buds, efficient taste-masking techniques (e.g., coating, complexation) are necessary to ensure patient compliance. Oral Disintegrating Mini Tablets integrate the stability of solid dosage and the ease of administration of liquids, making them an innovative solution for various patient groups [22].
Gastro-retentive (Floating) mini tablets
Gastro-retentive or floating mini tablets are to extend gastric residence time to enhance the bioavailability of drugs which are absorbed mainly from the stomach or proximal small intestine. Mini tablets are prepared with gas-generating agents such as sodium bicarbonate or calcium carbonate, usually in combination with swellable polymers. On interaction with gastric fluids, CO₂ is liberated and entrapped in the hydrocolloid matrix, and thus the mini tablets become buoyant. Such systems have been successful in the delivery of drugs such as Levodopa by utilizing 3 mm core mini tablets that are coated with Eudragit RL30D for prolonged release [23].
Bio-adhesive vaginal mini tablets
Traditional vaginal preparations (creams, ointments, gels) are plagued with leakage, low residence time, and messiness, resulting in decreased patient compliance. Bio-adhesive mini tablets provide a solid, accurate, and patient-compliant option. Prepared with bio-adhesive polymers, bio-adhesive mini tablets stick to the vaginal mucosa and provide localized, controlled drug release. By placing several mini-tablets along the vaginal cavity, consistent drug coverage and enhanced therapeutic effectiveness can be obtained. Hiorth et al.'s study proved the formation of bio-adhesive Hexyl Aminolevulinate (HAL) microtablets for cervical cancer photodynamic therapy, overcoming the issues of instability encountered with Hexyl Aminolevulinate (HAL) thermogels [7, 24].
Biphasic mini tablets
Biphasic mini tablets are formulated to release in a two-phase manner: an immediate burst release for quick action at the therapeutic site, with subsequent sustained release phase to sustain plasma levels of the drug within the therapeutic range. This minimizes the dosing frequency and increases compliance. These devices are particularly suitable for drugs such as Nonsteroidal Anti-Inflammatory Drugs, antihypertensives, antihistamines, and analgesics, wherein a rapid effect with sustained action is required. Biphasic release is possible by placing immediate-release excipients inside the pores of the mini-tablet matrix or by coating specific mini tablets with polymers having delay in drug release [17, 20].
Methods of producing mini tablets
Mini tablets, having a size range of 2–5 mm, are manufactured employing different traditional and modern pharmaceutical manufacturing processes. These processes are modified and optimized to ensure precision, uniformity, and target release characteristics in the small unit dosage forms. The dominant methods are:
Direct compression technique
A cost-efficient and effective technique where Active Pharmaceutical Ingredient (API) and excipients are compressed directly into mini-tablets without granulation. Advantages are fewer processing steps, shorter production time, negligible heat and moisture exposure, and less stability problem compared to wet granulation. This method is best when drug and excipients have good flowability and compressibility and not sensitive to moisture [21].
Wet granulation process
Here, crosslinked polymers are wetted out in water along with excipients and Active Pharmaceutical Ingredient (API), and a binder solution (generally polyvinylpyrrolidone) is added to produce granules, which are dried and compressed into mini-tablets. This enhances content uniformity and tablet hardness, particularly suitable for poorly flowing or low-dose drugs, but is more steps and more moisture and heat stability issues.
Table 4: Classification of mini tablets based on function and application
| Type | Description | Applications | References |
| Pediatric mini tablets | Small size, easy swallowing, taste-masked, accurate dosing | Pediatric therapy across all drug classes | [22] |
| Oral disintegrating mini tablets | Rapid disintegration in mouth, no water needed, taste-masked | Pediatrics, geriatrics, dysphagia patients | [22, 23] |
| Gastro-retentive mini tablets | Float in gastric fluids, prolonged stomach residence | Levodopa, metformin, antibiotics with stomach absorption | [23] |
| Bio-adhesive vaginal mini tablets | Localized retention, bioadhesive polymers, sustained release | Antimicrobials, hormonal therapy, anticancer drugs | [23, 24] |
| Biphasic mini tablets | Dual-phase release (immediate+sustained), precise plasma level control | NSAIDs, antihypertensives, antiallergics, chronic pain management | [24] |
Dry granulation method
Suitable for moisture-and heat-sensitive drugs, it includes compaction of dry powder mixtures in a chilsonator or roller compactor into ribbons, which are milled and sieved to make granules that are compressed into mini-tablets. It enhances stability and avoids solvent or drying, but needs to be optimized carefully for compaction parameters [15].
Melt-extrusion technique
It is an excipient-free process of pre-mixing Active Pharmaceutical Ingredient (API) with hot-melt extrusion excipients, charging the mixture to a melt-extruder, and processing at temperature, screw rate, and feed rate. Extrudates are chilled, milled, sieved, and compressed into mini-tablets. It is easy for the formulation of solid dispersions, improving solubility and bioavailability, especially for poorly water-soluble drugs [25].
Encapsulated mini-tablet systems
Encapsulated mini-tablet systems are made up of an array of mini-tablets—each of which can have a separate release profile-encapsulated within a hydroxypropyl methylcellulose (HPMC) capsule. They are most typically a mixture of immediate-release mini-tablets (IRMTs) and sustained-release mini-tablets (SRMTs). Upon breakup of the capsule, the mini-tablets are released independently, which enables modular dosing, variable drug release profiles, and combination therapy. All these provide a significant improvement in patient compliance, flexibility of dosing, and individualization of drug release kinematics [18].
Coating techniques: enteric and functional coatings
Mini-tablets tend to be coated using specific equipment like modified coating pans or fluidized bed coaters. Enteric coatings are increasingly used for the protection of acid-labile drugs against the gastric environment and to guard against gastric irritation. Such coatings are used to facilitate drug release mostly in the small intestine, where pH levels between 6.5 and 7.5. The most frequently employed enteric polymers are cellulose acetate phthalate, hydroxypropyl methylcellulose phthalate (HPMCP), shellac, waxes, fatty acids, and vegetable fibers. The enteric-coated drugs have the prefix "EC" in their names. Site-specific delivery of drugs using the method makes the drug more therapeutically active and reduces the systemic side effects [17, 21, 26].
Table 5: Summary of manufacturing methods for mini tablets
| Method | Features | Suitable for | References |
| Direct compression | Simple, fast, no granulation; requires good flow and compressibility | Moisture-stable APIs with suitable excipients | [21] |
| Wet granulation | Binder solution used; enhances flowability and compactibility | Low-dose, poorly flowing, or cohesive APIs | [22] |
| Dry granulation | No solvent or heat; suitable for sensitive APIs; uses roller compactor | Moisture/heat-sensitive APIs needing strong compacts | [23] |
| Melt-extrusion | Solvent-free; suitable for poorly soluble drugs; improves dissolution | BCS Class II/IV drugs, solid dispersions | [24] |
| Encapsulation | Multiple mini-tablets with varied release profiles packed in one capsule | Combination therapy, biphasic or modular release systems | [25] |
| Coating techniques | Enteric/functional coatings using fluidized bed or pan coating | Site-specific release, taste-masking, stability enhancement | [26] |
Preformulation studies mini-tablets
Preformulation is an important research step carried out before the dosage form formulation. It is meant to define the physicochemical attributes of the drug substance and assist in the selection of suitable excipients for the formation of an effective, stable, and producible product. The studies supply important knowledge about the drug's behavior under conditions of study, enabling rational dosage form design. In the case of mini-tablets, preformulation studies confirm the flowability, compressibility, and compatibility of the drug-excipient blend. The following preformulation parameters were studied for the formulated mini-tablet formulations [17].
Angle of repose
The angle of repose is a qualitative measure of the flow characteristics of powders. It is calculated from the fixed funnel test, where the powder is permitted to flow under gravity from a fixed height (h) through a fixed funnel onto a horizontal plane and forms a conical heap with a radius (r).
θ = tan-1 (h/r)
Where, θ is the angle of repose, ‘h’ is height of pile, ‘r’ is radius of base of the pile.
Lower angles (≤30°) generally point towards good flow properties, but higher angles point towards poor flow [15].
Bulk density and tapped density
These are utilized to assess the powder blends' ability to pack and compress.
Bulk Density= Weight of powder/Bulk volume
Tapped Density= Weight of powder/Tapped volume
Procedure: The powder was poured about 2 g gently into a 10 ml graduated cylinder. Tapping was done from 2.5 cm height at 2-second interval intervals until there was no volume change observed. Densities were determined by respective formulae [13, 15].
Compressibility Index (Carr's Index)
Carr's Index analyzes the compressibility and flow characteristics of powders. It is calculated with the equation:
Carr’s index (%) = [(Tapped Density-Bulk Density) * 100]/Tapped Density [30]
Hausner's Ratio
Hausner's Ratio is another flowability measurement, which is measured as:
Hausner’s ratio = TBD/Bulk Density [31]
Drug-excipient compatibility studies
Drug-excipient compatibility tests play an essential role during the preformulation stage to guarantee chemical stability and integrity of the final product. Fourier Transform Infrared Spectroscopy (FT-IR) and Differential Scanning Calorimetry (DSC) were used as the two techniques for the analysis of potential interactions.
Fourier transform infrared spectroscopy (FT-IR)
For FT-IR investigations, the spectra of the neat drug and the best mini-tablet formulations were obtained using the KBr pellet technique in Shimadzu FTIR-8600 spectrophotometer (Japan). The reason why there were no considerable differences in the peak heights was that there was no interaction of the drug with excipients chemically [32]. This establishes that chosen excipients are drug-compatible and appropriate for mini-tablet manufacturing.
Differential scanning calorimetry (DSC)
Differential Scanning Calorimetry (DSC) was carried out to identify possible physicochemical interactions and thermal characteristics of the drug in the formulation. Around 5 mg of sample was precisely weighed. Sealed in aluminum pans, the samples were scanned from 50 °C to 300 °C at 10 °C/min on a Shimadzu DSC-60 thermal analyzer. Calibration was done with indium and an empty sealed pan was taken as reference. Maintenance of the drug melting endotherm within the formulation indicated lack of interaction with excipients [32].
Table 6: Flow properties based on preformulation
| Angle of repose (°) | Carr’s index (%) | Hausner’s ratio | Flow properties | Reference |
| 25–30 | <10 | 1.00–1.11 | Excellent | [13] |
| 31–35 | 11–15 | 1.12–1.18 | Good | [15] |
| 36–40 | 16–20 | 1.19–1.25 | Fair | [30] |
| 41–45 | 21–25 | 1.26–1.34 | Passable | [30] |
| 46–55 | 26–31 | 1.35–1.45 | Poor | [31] |
| 56–65 | 32–37 | 1.46–1.59 | Very Poor | [31] |
| >66 | >38 | >1.60 | Very Very Poor | [31] |
Evaluation of mini-tablets
Mini-tablet formulations prepared from different concentrations and solvents were analyzed for various pharmaceutical evaluation parameters to ascertain quality, reproducibility, and patient acceptability. The following tests were conducted according to pharmacopeial guidelines [33–41]:
Weight Variation
The consistency of mini-tablet weight is important in ensuring dose accuracy. Twenty mini-tablets were individually taken at random from each batch and weighed on a calibrated analytical balance. The average weight was computed, and the weight of each tablet was compared with the average to calculate the percentage deviation.
Table 7: The USP/BP specifications require the following acceptable weight variation
| USP Specification: weight of tablet (mg) | BP specification: weight of tablet (mg) | Allowed percentage weight deviation (±%) | Reference |
| 130 or less | 80 or less | 10% | [33] |
| 130–324 | 81–250 | 7.5% | [33] |
| More than 324 | 251 or more | 5% | [33] |
A variation within the set range signifies adequate weight uniformity [33].
Hardness
Tablet hardness is an indication of the mechanical strength of the preparation. Six mini-tablets from every batch were examined with a Pfizer hardness tester, and values were quantified in terms of kg/cm². Mean and SD were estimated to determine mechanical integrity consistency [33–37].
Thickness
The measurement of the thickness of ten randomly chosen mini-tablets from each batch was carried out employing a digital vernier caliper (Mitutoyo Digimatic Caliper, Japan) and a screw gauge. The values were obtained in millimetres, and the mean±SD was expressed [38].
Friability
Friability measures resistance to abrasion upon handling. Twenty dust-free mini-tablets were weighed (W₁), filled into a Veego friabilator, and rotated at 25 rpm for 4 min (100 revolutions). After removing the dust, the final weight (W₂) was recorded. Percent friability was calculated as:
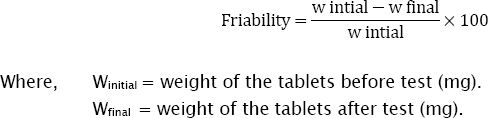
% Friability of mini-tablets less than 1% is considered acceptable [39].
Drug content uniformity
To find the uniform distribution of the active pharmaceutical ingredient (API):
Five mini-tablets were crushed and weighed, and an equivalent quantity of 10 mg of drug was taken and transferred to 100 ml of dissolution medium to provide a 100 μg/ml solution. 15 ml of this solution was diluted further up to 100 ml to obtain a 15 μg/ml working solution. Absorbance was recorded from the UV-visible spectrophotometer at the drug's specific wavelength. This provides dose uniformity within pharmacopeial specifications [40, 41].
Disintegration time
Disintegration time was evaluated for core mini-tablets with IP-defined disintegration test apparatus: A single tablet was put into each of the six tubes of the basket rack. A disk was introduced into each tube, and the basket was placed into 900 ml of distilled water at 37 °C±2 °C. The assembly was run at 30 cycles per minute.
The disintegration time for complete breakdown without any visible residue was noted. Decrease in disintegration time indicates greater drug release capacity, particularly for immediate-release mini-tablets [42, 43].
In vitro drug release
United States Pharmacopeia (USP) Type I (basket-type) dissolution apparatus was employed for studying drug release: Medium: 0.1 N HCl (pH 1.2) for 2 h (to mimic gastric environment). Phosphate buffer (pH 6.8) for the remaining 10 h (to mimic intestinal environment). Conditions: 900 ml medium, 100 rpm, at 37±0.5 °C Sampling: 5 ml withdrawn at fixed time intervals and replaced with same volume of fresh medium. Analysis: Release of drug was measured by UV spectrophotometry at the drug's specific λmax. In this study, release kinetics and suitability of the mini-tablets for immediate or controlled release profile is determined [44, 45].
Table 8: List of mini tablets available in the market
| Generic name | Brand name | References |
| Donepezil hydrochloride | Aricept | [33] |
| Levonorgestrel and Ethinyl Estradiol | Alesse | [33] |
| Sumatriptan and Naproxen Sodium Tablets | Treximet | [33] |
| Pancrelipase | Ultresa | [33] |
| Zafirlukast | Accolate | [33] |
| Galantamine HBr ER | Razadyne ER | [33] |
| Hydromorphone Hydrochloride Extended Release Tabs | Exalgo | [33, 38] |
| Warfarin Sodium | Coumadin | [33] |
| Fenofibric Acid Capsules | Trilipix | [9, 30] |
| Vorapaxar Tablets | Zontivity | [26] |
| Prasugrel Tablets | Effient | [26] |
| Olanzapine | Zyprexa, Zyprexa Zydis | [22] |
CONCLUSION
Mini-tablet development and use are a revolutionary leap forward in pharmaceutical dosage form design, with many biopharmaceutical, pharmacokinetic, and patient-friendly advantages. These systems of multiple units have several advantages over traditional single-unit tablets because of their even distribution in the gastrointestinal tract, which provides a consistent drug release, reduces inter-and intra-subject variability, and prevents dose dumping and gastric irritation. Mini-tablets allow accurate dose titration and are readily combinable for combination therapy, so they are effective for treating chronic diseases involving multi-drug regimens. Their modularity allows integration of various mini-tablets with distinct drug release profiles (e.g., immediate-release, sustained-release, or enteric-coated units) into one capsule, thus allowing for targeted and timed delivery of the drug. Modularity also permits tailoring according to patient requirements, including age, disease severity, and pharmacogenetic heterogeneity. In production, mini-tablets provide better content uniformity, reduced friability, and mechanical strength because of their small size and optimized compaction parameters. Production is compatible with standard tablet press machinery using adapted tooling, and the use of sophisticated coating methods, including fluidized bed coating, enables efficient functionalization (e.g., pH-sensitive or bioadhesive coatings). Pharmacologically, mini-tablets are most useful for drugs that have a limited absorption window or site-specific drug release needs, particularly in the case of the small intestine. Their size guarantees rapid gastric emptying and consistent intestinal transit, which enhances drug bioavailability and therapeutic efficacy. In addition, the use of mucoadhesive mini-tablets enhances the residence time of the drug at the absorption site even further, providing better performance in transmucosal or local delivery systems. Mini-tablets find broad application in clinical practice as a favored drug dosage form for children and elderly adults, many of whom struggle to swallow bulky tablets or capsules. Their ease of swallowing, dose flexibility, and simplicity of administration (e. g., sprinkling on food or liquid suspension) facilitate increased medication compliance and patient satisfaction. In summary, mini-tablets fill the gap between the requirement for accuracy dosing, improved drug release control, and patient-focused drug delivery, making them a critical technology in advancing personalized medicine and contemporary pharmaceutics.
ACKNOWLEDGMENT
This study was partially supported by from Mata Gujri University, Kishanganj, Bihar, India
FUNDING
Nil
AUTHORS CONTRIBUTIONS
Conceptualization: Bishal Sarkar, Data curation: Bishal Sarkar, Formal analysis: Bishal Sarkar, Investigation: Bishal Sarkar, Methodology: Bishal Sarkar, Resources: Bishal Sarkar, Supervision: Bishal Sarkar, Validation: Bishal Sarkar, Visualization: Bishal Sarkar, Writing–original draft: Bishal Sarkar, Writing–review and editing: Bishal Sarkar
CONFLICT OF INTERESTS
Authors declare that there is no conflict of interests.
REFERENCES
Banker GS, In ANR. The theory and practice of industrial pharmacy. 3rd ed Lachman L, Lieberman HA, Kanig JL, editors. Philadelphia: Lea & Febiger; 1991. p. 293.
Lennartz P, Mielck JB. Minitabletting: improving the compactability of paracetamol powder mixtures. International Journal of Pharmaceutics. 1998;173(1-2):75-85. doi: 10.1016/S0378-5173(98)00206-3, PMID 9871234.
Mitra B, Chang J, Wu SJ, Wolfe CN, Ternik RL, Gunter TZ. Feasibility of mini-tablets as a flexible drug delivery tool. Int J Pharm. 2017;525(1):149-59. doi: 10.1016/j.ijpharm.2017.04.037, PMID 28432019.
Sastry SV, Nyshadham JR, Fix JA. Recent technological advances in oral drug delivery a review. Pharm Sci Technol Today. 2000;3(4):138-45. doi: 10.1016/S1461-5347(00)00247-9, PMID 10754543.
Biradar SS, Bhagavati ST, Kuppasad IJ. Fast dissolving drug delivery systems: a brief overview. Internet J Pharmacol. 2006;4(2).
Katakam VK, Reddy S, Panakanti PK, Yamsani MR. Design and evaluation of a novel gas formation-based multiple-unit gastro retentive floating drug delivery system for quetiapine fumarate. Trop J Pharm Res. 2014;13(4):489-96. doi: 10.4314/tjpr.v13i4.1, PMID 30123456.
Igwe JC, Emenike IV, Oduola AR. Formulation and evaluation of finasteride sustained release matrix tablets using different rate-controlling polymers. Univ J Pharm Res. 2016;1(2):25-31. doi: 10.22270/ujpr.v1i2.R3.
Tawfeek HM, Saleem IY, Roberts M. Dissolution enhancement and formulation of rapid-release lornoxicam mini-tablets. J Pharm Sci. 2014;103(8):2470-83. doi: 10.1002/jps.24073, PMID 24995853.
Tehseen N, Rao V, Hadi MA. Design and characterization of twice daily mini-tablet formulation of pregabalin. Int J Pharm Pharm Sci. 2013;5(1):168-75.
Mastoi SM, Ali A, Aslam H, Niaz K. Comparison of antidyslipidemic potential of 80 mg of fenofibrate with 8 g of Nigella sativa seeds daily. Univ J Pharm Res. 2017;2(6):50-2.
Mohamed FA, Roberts M, Seton L, Ford JL, Levina M, Rajabi Siahboomi AR. Film-coated matrix mini-tablets for the extended release of a water-soluble drug. Drug Dev Ind Pharm. 2015;41(4):623-30. doi: 10.3109/03639045.2014.891128, PMID 24564797.
Keerthi ML, Kiran RS, Rao VU, Sannapu A, Dutt AG. Pharmaceutical mini-tablets: its advantages, formulation possibilities and general evaluation aspects: a review. Int J Pharm Sci Rev Res. 2014;28(1):214-21.
Mahajan KV, Akarte AM, Sapate MK, Baviskar DT, Jain DK. Designing and evaluation of compressed mini-tablets of ramipril as a biphasic delivery system. Indo Am J Pharm Res. 2013;3(9):7277-8.
Lopes CM, Sousa Lobo JM, Costa P, Pinto JF. Directly compressed mini matrix tablets containing ibuprofen: preparation and evaluation of sustained release. Drug Dev Ind Pharm. 2006;32(1):95-106. doi: 10.1080/03639040500388482, PMID 16455608.
Pogula AH, Nazeer S. Extended release formulation. Int J Pharm Technol. 2010;2(2):625-84.
Modi SA, Gaikwad PD, Bankar VH, Pawar SP. Sustained release drug delivery system: a review. Int J Pharm Res Dev. 2011;2(11):147-98.
C Shaikh SC, Sanap D, Bhusari DV, Jain S, Kochar PP, Sanchati VN. Formulation and evaluation of ibuprofen gastro-retentive floating tablets. Univ J Pharm Res. 2018;3(4):20-5. doi: 10.22270/ujpr.v3i4.178.
Shah BA, Patel AS, Patel BJ, Patel DJ, Qu A. Mini-tablet drug delivery system for pediatric dosage form: a review of manufacturing perspectives. Int J Drug Dev Res. 2018;10(3):47-52.
Lopes CM, Lobo JM, Pinto JF, Costa P. Compressed mini-tablets as a biphasic delivery system. Int J Pharm. 2006;323(1-2):93-100. doi: 10.1016/j.ijpharm.2006.05.063, PMID 16828999.
Rao NG, Hadi MA, Panchal H. A novel approach to sustained montelukast sodium release: differentially coated mini-tablets in HPMC capsules. Int J Pharm Biomed Sci. 2011;2(2):90-7.
Singh S, Virmani T, Virmani R, Mahlawat G, Kumar P. Fast dissolving drug delivery systems: formulation preparation techniques and evaluation. Univ J Pharm Res. 2018;3(4):60-9. doi: 10.22270/ujpr.v3i4.185.
Klingmann V, Seitz A, Meissner T, Breitkreutz J, Moeltner A, Bosse HM. Acceptability of uncoated mini-tablets in neonates a randomized controlled trial. J Pediatr. 2015;167(4):893-896.e2. doi: 10.1016/j.jpeds.2015.07.010, PMID 26259675.
Opeyemi OT, Adegbenro OO. Development and characterization of direct compressed matrix mini-tablets of naproxen sodium. Univ J Pharm Res. 2018;3(5):7-11. doi: 10.22270/ujpr.v3i5.205.
Karthikeyan D, Vijayalaxmi A, Santhosh Kumar C. Formulation and evaluation of biphasic delivery system of aceclofenac mini-tablets in hard gelatin capsules. Int J Novel Trends Pharm Sci. 2013;3(2):39-45.
Solanki B, Patel R, Barot B, Parejiya P, Shelat P. Multiple unit dosage forms: a review. Pharmtechmedica. 2012;1(1):11-21.
Nweje Anyalowu PC. Design and evaluation of a chronotherapeutic pulsatile drug delivery system of cilnidipine. UJPR. 2017;2(5):18-22. doi: 10.22270/ujpr.v2i5.R4.
Bodea M, Tomuta I, Leucuta S. Identification of critical formulation variables for obtaining metoprolol tartrate mini-tablets. Farmacia. 2010;58(6):719-27.
Chauhan V. Fast dissolving tablets: a promising approach for drug delivery. UJPR. 2017;2(4):58-64. doi: 10.22270/ujpr.v2i4.RW4.
Garg D, Saini V, Gupta S, Kapoor DN, Joshi L. Controlled release multiple units and single-unit doses: a literature review. DHR Int J Pharm Sci. 2013;4(2):66-73.
Rosenson RS. Low high-density lipoprotein cholesterol and cardiovascular disease: risk reduction with statin therapy. Am Heart J. 2006;151(3):556-63. doi: 10.1016/j.ahj.2005.03.049, PMID 16504615.
Zhu T, Ansquer JC, Kelly MT, Sleep DJ, Pradhan RS. Comparison of the gastrointestinal absorption and bioavailability of fenofibrate and fenofibric acid in humans. J Clin Pharmacol. 2010;50(8):914-21. doi: 10.1177/0091270009354995, PMID 20145261.
Chen Y, Qiu Y, Reiland TL. Pharmaceutical compositions comprising effervescent agents and fenofibrate. United States Patent Application US20100021393. Vol. A1; 2010.
Venkat Tumuluri. Pharmaceutical mini-tablets. In: Drug delivery trends. Amsterdam: Elsevier; 2020. p. 123-39. doi: 10.1016/B978-0-12-817870-6.00006-7.
Vogt M, Kunath K, Dressman JB. Dissolution enhancement of fenofibrate by micronization cogrinding and spray-drying: comparison with commercial preparations. Eur J Pharm Biopharm. 2008;68(2):283-8. doi: 10.1016/j.ejpb.2007.05.010, PMID 17574403.
Gundu RK, Gali VR, Deshpande A, Reddy PS. Formulation and evaluation of sustained-release matrix tablets of fenofibrate. Int J Pharm Sci Res. 2015;6(5):2105-12. doi: 10.13040/IJPSR.0975-8232.6(5).2105-12.
Sahni J, Raj S, Ahmad FJ, Khar RK. Design and in vitro characterization of buccoadhesive drug delivery system of insulin. Indian J Pharm Sci. 2008;70(1):61-5. doi: 10.4103/0250-474X.40333, PMID 20390082.
Al Ameri MN, Nayuni N, Anil Kumar KG, Perrett D, Tucker A, Johnston A. The differences between the branded and generic medicines using solid dosage forms: in vitro dissolution testing. Results Pharma Sci. 2012;2:1-8. doi: 10.1016/j.rinphs.2011.12.001, PMID 25755988.
Sampath K. Method development and validation of pravastatin sodium in human plasma by using LCMS/MS. JBB. 2011;3(3). doi: 10.4172/jbb.1000057.
Patil P, Joshi P, Paradkar A. Effect of formulation variables on preparation and evaluation of gelled self-emulsifying drug delivery system (SEDDS) of ketoprofen. AAPS PharmSciTech. 2004;5(3):e42. doi: 10.1208/pt050342, PMID 15760075.
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C. DDSolver: an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010;12(3):263-71. doi: 10.1208/s12248-010-9185-1, PMID 20373062.
Reza MS, Quadir MA, Haider SS. Comparative evaluation of plastic hydrophobic and hydrophilic polymers as matrices for controlled-release drug delivery. J Pharm Pharm Sci. 2003;6(2):282-91. PMID 12935440.
Dhas SK, Deshmukh G. Formulation and evaluation of meloxicam microspheres for colon-targeted drug delivery. Asian J Pharm Clin Res. 2021 Aug;14(8):45-51. doi: 10.22159/ajpcr.2021.v14i8.38482.
Ashwin Kumar K, Rathnam G. Development and evaluation of controlled porosity osmotic tablets of candesartan cilexetil using inclusion complex system. Asian J Pharm Clin Res. 2025 Jan;18(1):46-51. doi: 10.22159/ajpcr.2025v18i1.53194.
Raj R, Kolay A, Havelikar U. A review on solid lipid nanoparticles. Int J Curr Pharm Sci. 2023 Sep;15(5):10-6. doi: 10.22159/ijcpr.2023v15i5.3051.
Hemalatha B, Ramu A, Vidyadhara S. Formulation and evaluation of azelnidipine fast-dissolving tablets. Int J App Pharm. 2025;17(1):113-22. doi: 10.22159/ijap.2025v17i1.52398.